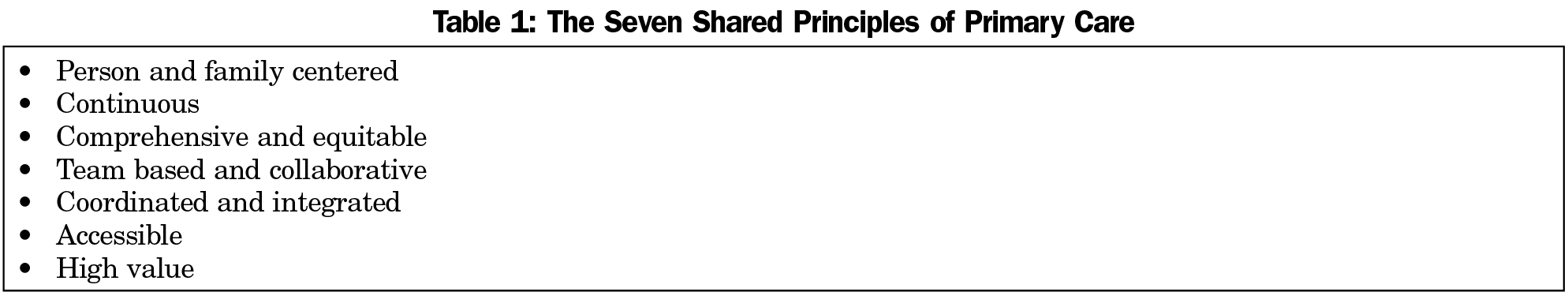
The seven Shared Principles are listed in Table 1. The collaborative process reidentified the four classic Starfield principles—continuous, comprehensive, coordinated, and accessible—along with several other important concepts. The complete text of the Shared Principles is included verbatim in Appendix 1 (https://journals.stfm.org/media/2045/epperly-appendix1.pdf); the list of endorsing organizations is online at https://www.pcpcc.org/principles/signers. Following are some of the most salient modifications and how they are different from other sets of primary care principles.
8 Primary Care
In this chapter, we will consider the topic of primary care and the central role primary care plays in achieving improved population health outcomes.
We will begin by watching a 30-minute round table discussion from 2008, highlighting the challenges facing primary care in the United States and why many believed primary care was in a state of “crisis” at the time.
We will then look at models to improve primary care currently being implemented: the “Shared Principles of Primary Care” introduced in 2019 and the “Key Attributes of Advanced Primary Care” introduced in December 2020. As you read over these materials, please think about how these emerging approaching to providing primary care aim to address some of the major issues facing primary care back in 2008, including:
- insufficient time for primary care physicians to adequately treat patients,
- low job satisfaction/high burnout among primary care physicians,
- fewer medical residents pursuing careers in primary care,
- patient difficulties accessing a suitable primary care provider, and
- patient dissatisfaction with the very short amount of time primary care providers were able to spend with them.
Also please consider how these emerging models place greater focus on prevention related to social and behavioral determinants of health.
Watch the New England Journal of Medicine “Redesigning Primary Care” Roundtable Discussion videos
This half-hour video (broken into four parts) presents a panel of experts discussing strategies to redesign primary care practice to make it more attractive to physicians and more beneficial to patients. This video was created in 2008, and you will recall seeing examples of some of the ideas that are mentioned being implemented (at least on a limited, preliminary basis) in content from prior modules. However, this video does a good job of covering some of the major issues primary care physicians have faced with our healthcare system for the last several decades.
The intended audience for this video is physicians and others familiar with health policy. Accordingly, some of the discussion may cover material with which you are not familiar. As you watch this video, focus on the specific items identified in the study guide. View the four parts of the video in sequential order.
To access the complete transcript for all four video parts, please use the Redesigning Primary Care video transcript link (Alternative link).
Click the Play icon to begin.
If video doesn’t appear, follow this direct link: Redesigning Primary Care, Part 1 (07:53 min.)Use the direct link above to open the video in YouTube to display the video captions and expand the video.
Redesigning Primary Care, Part 1 Video
Click the Play icon to begin.
https://youtube.com/watch?v=ZSrMyHKigdI%3Frel%3D0%26start%3D0
If video doesn’t appear, follow this direct link: Redesigning Primary Care, Part 1
Links to an external site. (07:53 min.)
Use the direct link above to open the video in YouTube to display the video captions and expand the video.
Redesigning Primary Care, Part 2 Video – New Delivery Models
Click the Play icon to begin.
If video doesn’t appear, follow this direct link: Redesigning Primary Care, Part 2 (09:15 min.)
Use the direct link above to open the video in YouTube to display the video captions and expand the video.
Redesigning Primary Care, Part 3 Video – Payment Reform
Click the Play icon to begin.
If video doesn’t appear, follow this direct link: Redesigning Primary Care, Part 3 (09:15 min.)
Use the direct link above to open the video in YouTube to display the video captions and expand the video.
Redesigning Primary Care, Part 4 Video – Revolution or Evolution?
Click the Play icon to begin.
If video doesn’t appear, follow this direct link: Redesigning Primary Care, Part 4 (06:02 min.)
Use the direct link above to open the video in YouTube to display the video captions and expand the video.
NEJMvideo. (2010, April 2). Redesigning Primary Care, Parts 1, 2, 3, and 4. YouTube.
Excerpts from the article: “The Shared Principles of Primary Care: A Multistakeholder Initiative to Find a Common Voice“
Next, please read the following excerpts from an article published in the medical journal Family Medicine, discussing the seven shared principles of primary care. As you complete this reading, please think about how these seven shared values build upon some of the concepts discussed in the “Redesigning Primary Care” roundtable discussed above.
(Note: You may recall the name of the lead author of this article, Dr. Tedd Epperly, from the “Fractured” video lecture you were assigned to watch earlier in the class. Dr. Epperly is the CEO of the Family Medical Residency of Idaho, has previously served as the president of the American Academy of Family Physicians, and is generally regarded as one of the leading experts on family medicine and primary care in the United States.)
Article citation:
Epperly, T., Bechtel, C., Sweeney, R., Greiner, A., Grumbach, K., Schilz, J., Stream, G., & O’Connor, M. (2019). The shared principles of primary care: a multistakeholder initiative to find a common voice. Family Medicine, 51(2), 179–184. https://doi.org/10.22454/FamMed.2019.925587
Ted Epperly, MD | Christine Bechtel, MA | Rosemarie Sweeney, MPA | Ann Greiner, MA | Kevin Grumbach, MD | Julie Schilz, MBA, BSN | Glen Stream, MD | Malachi O’Connor, PhD
Fam Med. 2019;51(2):179-184.
DOI: 10.22454/FamMed.2019.925587
Introduction and Rationale
All who work in the US health care system struggle to design a more effective, efficient, accessible, high-quality, and high-value enterprise.1,2 Primary care is widely acknowledged to be essential for better health and health care value and should be foundational to all health care systems.3-8 Many observers have pointed to the US health system’s underinvestment in primary care as an important reason for the nation’s lagging performance.3,9 Significant changes have occurred in the way primary care is organized, financed, and delivered in response to greater demand for high-quality services, rising health care costs, and increasing burden of disease across populations.10 Concepts such as the Patient Centered Medical Home emerged to describe a more advanced model of primary care.11,12 The ongoing transformation of primary care delivery models and heightened attention to the importance of primary care have prompted fresh thinking about the essential principles that define primary care. In this article, we present an updated primary care conceptual model, the Shared Principles of Primary Care, developed by a diverse group of stakeholders representing health professionals, consumers, purchasers, and health plans. We discuss the context for developing this updated set of principles, the process for drafting them, and the implications for policy and practice.
****
The Shared Principles
1. Person and Family Centered
The decision to replace “patient centered” with the term “person and family centered” was a very intentional one, responsive to concerns expressed by consumer advocates that the word “patient” objectified individuals in a sick or dependent role. The principles sought to move beyond the narrow framework of a disease care system to one promoting health. This first of the Shared Principles affirms an empowered partnership role for individuals and families. For example, the principle asserts that:
primary care is grounded in mutually beneficial partnerships among clinicians, staff, individuals, and their families, as equal members of the care team. Care delivery is customized based on individual and family strengths, preferences, values, goals, and experiences using strategies such as care planning and shared decision making. There are opportunities for individuals and their families to shape the design, operation, and evaluation of care delivery.
2. Continuous
This principle reiterates the longstanding precept that dynamic, trusted, respectful, and enduring relationships between individuals, families, and their clinical team members are hallmarks of primary care.
The secret sauce of primary care is the ongoing trusting relationship between clinicians and the primary care team and individuals and families that is a healing process unto itself. This allows the importance of a sustained incremental approach over time to be foundational to dealing with acute, chronic, behavioral, and prevention-based health care problems and issues.18
3. Comprehensive and Equitable
This principle emphasizes important contemporary aspects of comprehensive primary care, such as behavioral and mental health as well as oral health. Primary care serves all ages, both genders, and the majority of health care problems. The principle also ties comprehensiveness to emerging concepts in health equity, calling on primary care to:
seek out the impact of social determinants of health and societal inequities. The more comprehensive the skill set and scope of practice is in the existing clinic setting the higher the percentage of problems that can be cared for in the primary care setting. Primary care practices are also recognizing the importance of the social determinants of health and linking patients who have social determinate issues (eg, food insecurity, transportation issues) with community resources that can further work with them to resolve these issues. Primary care practices partner with health and community-based organizations to promote population health and health equity, including making inequities visible and identifying avenues for solution.
Current research demonstrates that health care influences only approximately 10%-20% of a person’s health, with a person’s behaviors, environment, genetic makeup, and social conditions being the most powerful determinants of health, illness, and death.19
4. Team Based and Collaborative
This principle affirms that individuals and families are critical members of primary care teams. In recognizing the multidisciplinary nature of team-based care, it also asserts that health care professional members of the team are trained to work together at the top of their skill set, according to clearly defined roles and responsibilities.
This principle broadens the importance of relationships to include the entire primary care team. Many team members, from nurses, medical assistants, receptionists, social workers, nutritionists, and clinicians, form relationships with the persons and families cared for by the practice. All primary health care team members are important in the delivery of team-based collaborative care. This distribution of workload across the team is fundamental to decreasing clinician and health care team member burnout and increasing the joy in practice.
5. Coordinated and Integrated
The Shared Principles largely reiterate the central emphasis on contemporary issues such as “transitions of care to achieve better health and seamless care delivery across the life span.” The term “integrated” refers to how the individual’s health data and records can inform care within the primary care team and with other health care professionals in the medical neighborhood. The term “coordinated” refers to how health care is seamlessly arranged with others participating with the individual’s care outside of the primary care practice in the medical neighborhood. With the emergence of evolving health information technology, new and dynamic ways of integrating and coordinating health care information and data can be performed both synchronously and asynchronously with individuals to optimize their health care and health.
6. Accessible
This principle acknowledges the changing nature of access in a digital communication era, asserting that:
primary care is readily accessible, both in person and virtually for all individuals regardless of linguistic, literacy, socioeconomic, cognitive, or physical barriers. This accessibility goes far beyond the concept of face-to-face visits. Meeting patients’ health and health care needs electronically, telephonically, and in other technologically empowered ways is both achieving person- and family-centered care and high-value accessible care. Primary care provides individuals with easy, routine access to their health information.
Moreover, person- and family-centered access means that “clinicians and staff are available and responsive when, where, and how individuals and families need them.”
7. High Value
This principle goes further than most prior formulations by asserting that primary care has responsibility for both quality and patient experience cost components of health care value, and once again highlights the importance of a person- and family-centered approach.
Primary care achieves excellent, equitable outcomes for individuals and families, including using health care resources wisely and considering costs to patients, payers, and the system. Primary care practices employ a systematic approach to measuring, reporting, and improving population health, quality, safety, and health equity, including partnering with individuals, families, and community groups.
Additionally, one cannot place enough value on the importance of the trusting relationship to drive quality and patient safety and to appropriately lower health care costs.
****
Conclusion
The United States health care system is at a critical crossroad in its transformation. The foundational importance of primary care in our future health care system cannot be overstated. The undertaking of the collaborative process of refocusing on the value of primary care by diverse stakeholders forming new partnerships both inside and outside of health care is fundamental to this effort. This shared process of principles creation across multiple stakeholders helps create a bonding covenant with our patients and the public.
This set of seven Shared Principles of Primary Care helps define the foundational importance of what primary care does to advance better health, a more satisfying health care experience, and more affordable costs. The Shared Principles were formulated with an understanding that they are aspirational. For them to be actualized consistently and robustly across the diverse landscape of primary care practices in the United States will require not just commitment from the primary care practice community, but also a willingness of the public, payers, and policy makers to prioritize primary care. With more than 300 organizational endorsers, the Shared Principles provide an opportunity for individuals and organizations committed to a vibrant primary care sector to speak with one voice about the bedrock elements of primary care and their importance to the health system. Although the specific ways of delivering primary care will continue to evolve as our complex health system changes, these core principles help to define the enduring essence and value of primary care.
(Please click here to access the full article and references (alternative link))
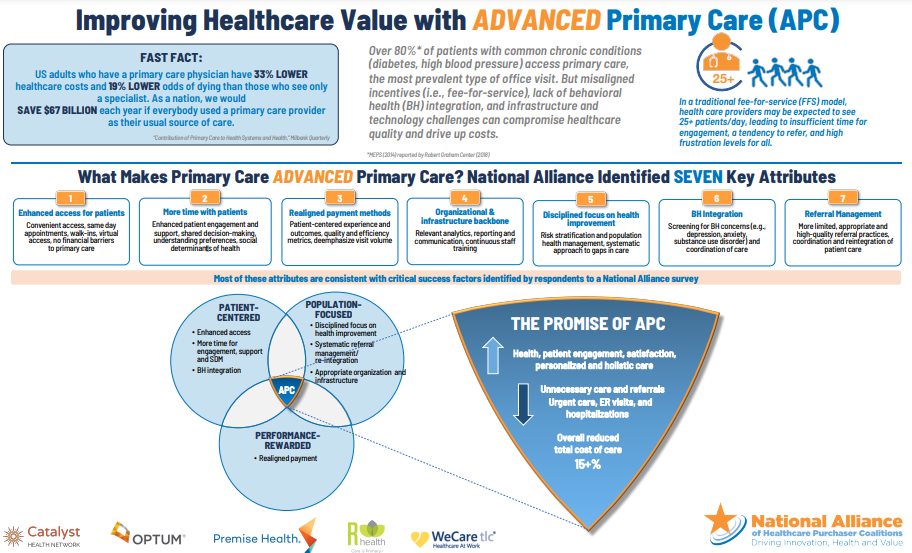
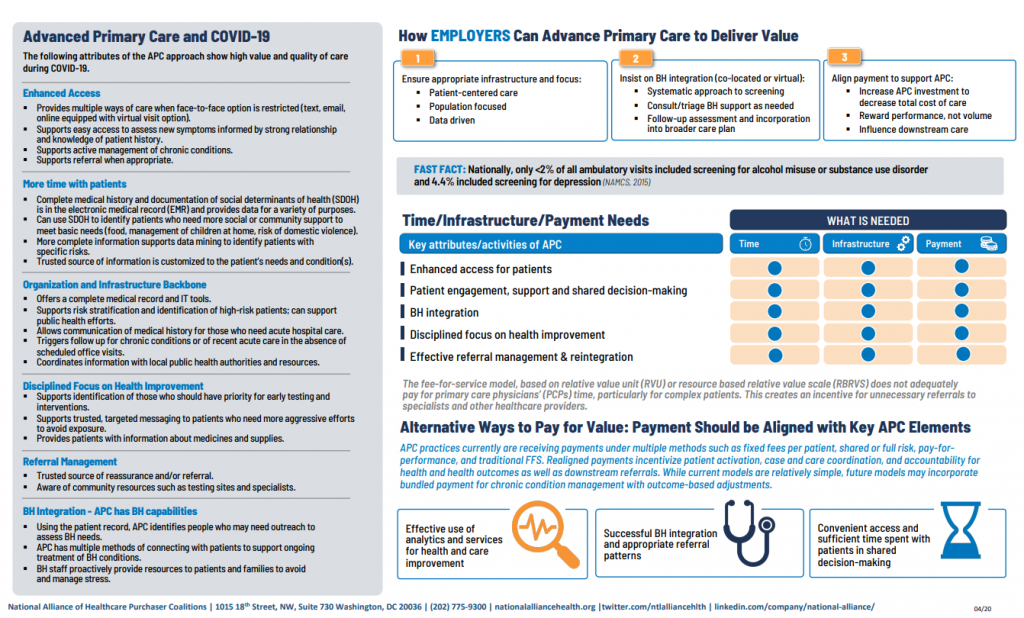
Improving Healthcare Value with ADVANCED Primary Care (APC) (Alternative Link)
- This infographic put together by the National Alliance of Healthcare Purchaser Coalitions, summarizes the seven key attributes of Advanced Primary Care, and how primary care based on these attributes contribute to better outcomes in healthcare delivery. For convenience, these seven attributes of APC also provided in the infographic are listed below:
- Enhanced access for patients: Convenient access, same-day appointments, walk-ins, virtual access, no financial barriers to primary care
- More time with patients: Enhanced patient engagement and support, shared decision-making, understanding preferences, social determinants of health
- Realigned payment methods: Patient-centered experience and outcomes, quality and efficiency metrics, deemphasize visit volume
- Organizational & infrastructure backbone: Relevant analytics, reporting and communication, continuous staff training
- Disciplined focus on health improvement: Risk stratification and population
health management, systematic approach to gaps in care - Behavioral Health (BH) Integration: Screening for BH concerns (e.g.,- depression, anxiety, substance use disorder) and coordination of care
- Referral Management: More limited, appropriate and high-quality referral practices, coordination and reintegration of patient care
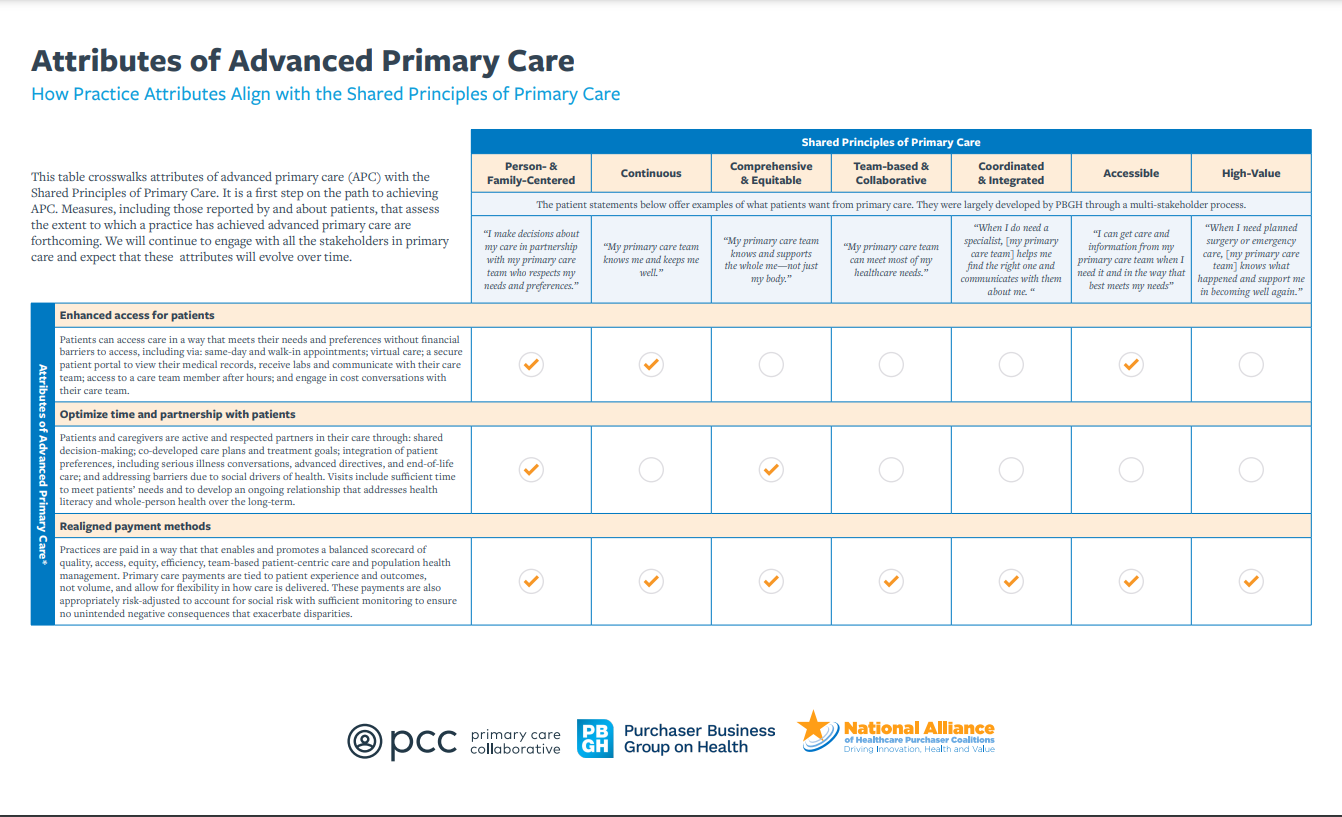
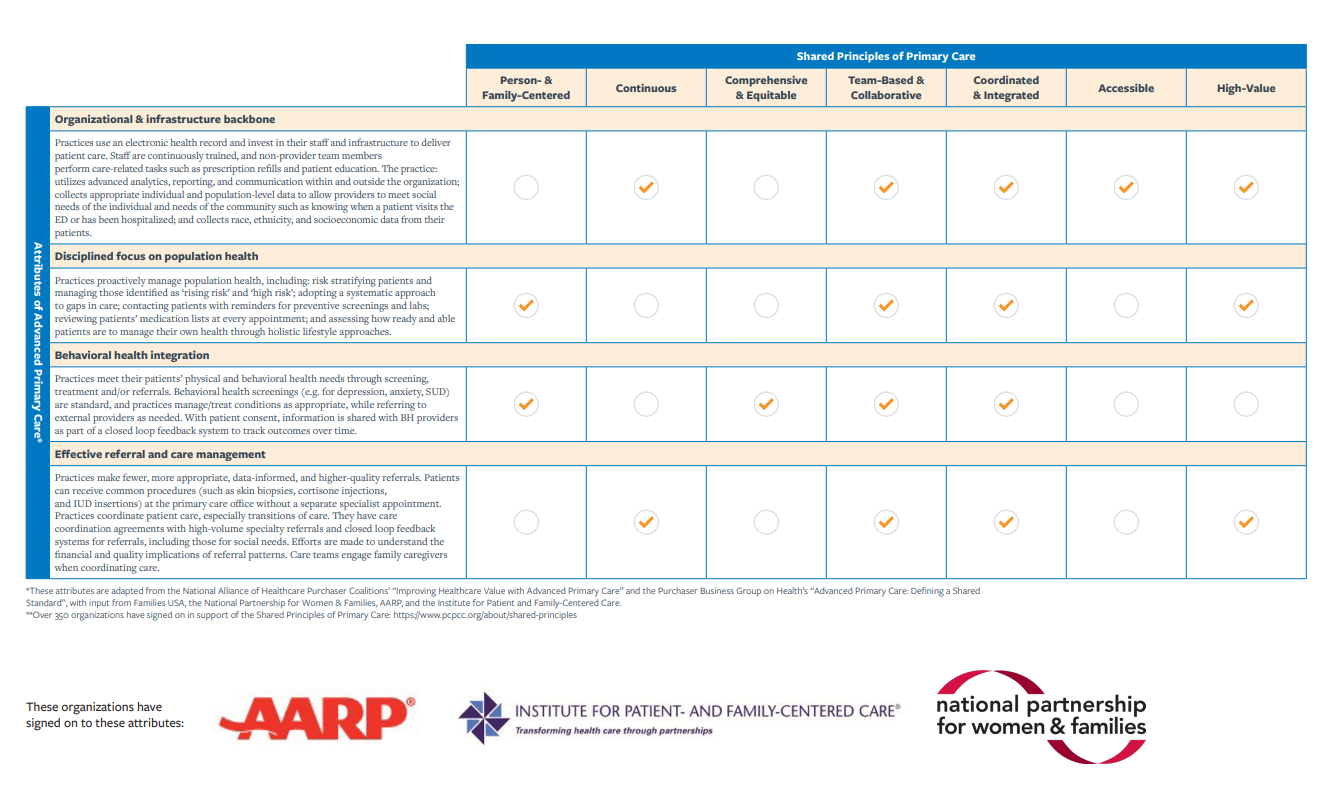
Attributes of Advanced Primary Care: How Practice Attributes Align with the Shared Principles of Primary Care (Alternative Link)
- This infographic illustrates how the Seven Attributes of Advanced Primary Care can be used to put into practice the Shared Principles of Primary Care discussed above in the article by Epperly et al. (2019).