14 Chapter 14 Exercise Design
Exercise Design
During this class you experienced a group exercise which is similar to a simple table top exercise. In the world of emergency response the use of exercises to test the effectiveness of an emergency plan is so critical. In fact it is so important that hospitals are required to conduct live exercises frequently.
Within an Emergency Management section there are planners who will put together an exercise to test the plan. The exercise may be to test just a part of the plan or the entire plan. FEMA has a week long in person Exercise Design class that they provide at their training facility in Emmitsburg Maryland.
One time here in Ada County there was an exercise to test the dispatch system and what would happen if the repeater for the radios failed on Shaffer Butte. Would you believe that this is what happened when the test was being conducted. The key was to find workarounds should this happen.
There was an instance in the Midwest where a community had an exercise at their airport around an airplane crash at the airport. Almost within the month the community actually experienced an airplane crash and because of the recent exercise they were more prepared.
Developing a good functional exercise that involves multiple agencies takes a lot of time and effort. It is not something that happens overnight. You must have good relationships with the entities that will be participating. This again is why the LEPC is so valuable. By spending time with the entities you know the people you will be working with to develop the plan.
The planner will go to teach of the entities that will be a “player” in the exercise and ask them what the entity hopes to get out of the exercise. The planner then develops specific objectives for that entity related to the exercise and inserts elements into the plan to test that objective. For example in Idaho the Local Health Districts are responsible for assessing the number of available beds in local hospitals during an emergency. The health districts had never tested if this would work. Therefore, it was written into the next mass injury/fatality exercise in Ada County. The process was that the State Bridge would set up a call with all of the hospitals and the local health district. The State Bridge called the hospitals and advised them that in 15 minutes where would be a bridge call with health district and that the hospitals were to have ready the number of available beds. The results was that it actually worked in the exercise so we could assume in a real situation it would work also.
A well developed plan creates the feeling within the group that is roll playing the various elements that this is really happening. I, Tom Turco, while attending the Exercise Design training class in Emmitsburg experience this personally. In the class the instructors will explain a principle of exercise design and then the attendees would actually participate in an exercise to stress the point of the training. During the training one of the attendees became absorbed in the roll they were playing that they started verbally attacking the others for not following the orders that were given. The exercise coordinator had to pull that person out of the room and tell them to “cool their jets” and remember that this was just an exercise and not real.
The state of California has developed templates for exercises for the counties to use. Below you will find the main template
You will also find the template for hospital objectives for an exercise. You will notice that the template for the hospital follows some of the capabilities we have been looking at in this class. In the exercise a hospital would not have to use all the objectives but could select some of them that they really wished to find out how they are doing related to the specific capability. As you go back in the class the main issues would be the items that were marked as priority in each of the capabilities we studied.
14.06 Assignment Worksheet-Exercise-Link to Canvas Site
In this exercise you will be a planner for a local health department. Your agency is in an area that receives persons from the western portion of Africa where Ebola is endemic. Your agency wishes to develop an exercise for your community around what to do if multiple people have entered your community and have later been diagnosed with Ebola and there have been deaths.
Ebola virus disease (EVD) is a deadly disease with occasional outbreaks that occur mostly on the African continent. EVD most commonly affects people and nonhuman primates (such as monkeys, gorillas, and chimpanzees). It is caused by an infection with a group of viruses within the genus Ebolavirus:
The virus first spreads to people through direct contact with the blood, body fluids and tissues of animals. Ebola virus then spreads to other people through direct contact with body fluids of a person who is sick with or has died from EVD. This can occur when a person touches these infected body fluids or objects that are contaminated with them. The virus then gets into the body through broken skin or mucous membranes in the eyes, nose, or mouth. People can get the virus through sexual contact with someone who is sick with or has recovered from EVD. The virus can persist in certain body fluids, like semen, after recovery from the illness.
The virus spreads through direct contact (such as through broken skin or mucous membranes in
- Blood or body fluids (urine, saliva, sweat, feces, vomit, breast milk, amniotic fluid, and semen) of a person who is sick with or has died from Ebola virus disease (EVD).
- Objects (such as clothes, bedding, needles, and medical equipment) contaminated with body fluids from a person who is sick with or has died from EVD.
- Infected fruit bats or nonhuman primates (such as apes and monkeys).
- Semen from a man who recovered from EVD (through oral, vaginal, or anal sex). The virus can remain in certain body fluids (including semen) of a patient who has recovered from EVD, even if they no longer have symptoms of severe illness. There is no evidence that Ebola can be spread through sex or other contact with vaginal fluids from a woman who has had Ebola.
When people become infected with Ebola, they do not start developing signs or symptoms right away. This period between exposure to an illness and having symptoms is known as the incubation period. A person can only spread Ebola to other people after they develop signs and symptoms of Ebola.
Additionally, Ebola virus is not known to be transmitted through food. However, in certain parts of the world, Ebola virus may spread through the handling and consumption of wild animal meat or hunted wild animals infected with Ebola. There is no evidence that mosquitoes or other insects can transmit Ebola virus.
Risk
- Health workers who do not use proper infection control while caring for Ebola patients, and family and friends in close contact with Ebola patients, are at the highest risk of getting sick. Ebola can spread when people come into contact with infected blood or body fluids.
- Ebola poses little risk to travelers or the general public who have not cared for or been in close contact (within 3 feet or 1 meter) with someone sick with Ebola.
Symptoms may appear anywhere from 2 to 21 days after contact with the virus, with an average of 8 to 10 days. The course of the illness typically progresses from “dry” symptoms initially (such as fever, aches and pains, and fatigue), and then progresses to “wet” symptoms (such as diarrhea and vomiting) as the person becomes sicker.
( https://www.cdc.gov/vhf/ebola/about.html)
Please Address the following questions:
- List at least 5 agencies or facilities in your community that you would want to participate in the exercise. ( Note: There are many more than 5 but this will be sufficient for this worksheet)
- List at least 3 objectives for the exercise (What do you wish to “test” in your community to see if they are ready to respond to threat of Ebola)
- What type of exercise would you wish to conduct and why?
- Would you anticipate opening up the Emergency Operations Center? Why or why not?
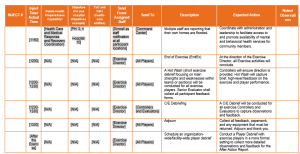
[INSERT YEAR]
STATEWIDE MEDICAL AND HEALTH EXERCISE[1]
PREFACE The [Insert year] California Statewide Medical and Health Exercise (SWMHE) is sponsored by the California Department of Public Health (CDPH) and the Emergency Medical Services Authority (EMSA). This Master Scenario Events List (MSEL) was produced with input, advice, and assistance from the SWMHE Planning Team, comprised of representatives from:
• California Ambulatory Surgery Association (CASA)
• California Association of Health Facilities (CAHF)
• California Department of Public Health (CDPH)
• California Emergency Medical Services Authority (EMSA)
• California Hospital Association (CHA)
• California Governor’s Office of Emergency Services (Cal OES)
• California Primary Care Association (CPCA)
• County of Riverside Emergency Management Department
• DaVita Dialysis
• Inland Counties Emergency Management Agency
• Kaiser Permanente
• Los Angeles County Healthcare Agency
• Mariposa County
• Napa County Emergency Medical Services Agency
• Sacramento County Emergency Medical Services Agency
• San Joaquin County Emergency Medical Services Agency
• Sharp HealthCare
• Sutter Medical Center
This MSEL follows guidelines set forth by the U.S. Federal Emergency Management Agency (FEMA) Homeland Security Exercise and Evaluation Program (HSEEP). This MSEL is a guidance document that can and should be modified by participating entities with the particulars of their exercise. It is a complementary document to other documents developed for this exercise, including the Exercise Plan. It is tangible evidence of [Jurisdiction/Organization/Facility]’s commitment to ensure public safety through collaborative partnerships that will prepare them to respond to any emergency. This MSEL provides staff with all the necessary injects and scenario updates to lead and conduct a full exercise. Only controllers and evaluators should view the MSEL. All exercise participants should use appropriate guidelines to ensure proper control of information within their areas of expertise and protect this material in accordance with current jurisdictional directives.
[CUSTOMIZING THE MSEL][This document serves as a template guidance document. This MSEL, and particularly the schedule and inject specifications, should be modified to reflect the unique characteristics of your region and participants. Bracketed text (e.g., [your jurisdiction]) is provided to aid with location-specific tailoring. These sections contain instructions, examples, or placeholders to facilitate completion of this document. These should be removed or modified as appropriate prior to finalizing this document. Additional detail regarding the SWMHE, to include several other supporting documents, are available for planners at https://www.cdph.ca.gov/Programs/EPO/Pages/swmhe_current.aspx].
ADMINISTRATIVE HANDLING INSTRUCTIONS1. The title of this document is the California Statewide Medical and Health Exercise (SWMHE) Program Master Scenario Events List (MSEL).
2. The information gathered in this MSEL is designated as For Official Use Only (FOUO) and should be handled as sensitive information that is not to be disclosed. This document should be safeguarded, handled, transmitted, and stored in accordance with appropriate security directives. Reproduction of this document, in whole or in part, without prior approval from [Jurisdiction/Organization/Facility] is prohibited.
3. For more information about the exercise, please consult the following points of contact (POCs):
Jurisdictional Exercise Point of Contact:
Name
Title, Agency
Street Address
City, State, Zip
Telephone
Exercise Support Team Point of Contact
Name
Title, Agency
Street Address
City, State, Zip
Telephone
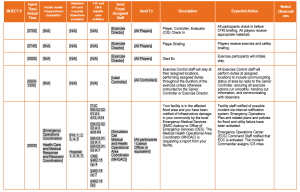
MASTER SCENARIO EVENTS LIST
[How To Use This Document: The scenario for this exercise is objective-driven; it was developed in order to fully test the suggested exercise objectives and core capabilities. If participating agencies decide to add or subtract from the suggested list of objectives, they are advised to review the scenario to confirm that the new objectives will be fully tested. Bracketed text (e.g., [your jurisdiction]) is provided to aid with location-specific tailoring. Additional resources are available for planners at https://www.cdph.ca.gov/Programs/EPO/Pages/swmhe_current.aspx]
Customizing the Scenario with Additional Components
- All jurisdictions should consider adding or revising the components of the scenario according to their objectives, participants, and most likely hazards. The following is a list of additional, optional components that your exercise planning team may consider adding:
- Water testing (Boil Water Notices, etc.)
- Local sanitation procedures (notify public)
- Health hazards related to standing water (contaminated water, hazards materials, power lines, etc.)
- Local Communicable Disease Plan policies and procedures
- Local laboratory testing and reporting protocols
- Personal Protective Equipment (PPE) recommendations and messaging to healthcare facilities (standing water, loss of water, etc.)
- Medical Examiner/Coroner’s Office involvement and roles
- Patient and/or Facility Evacuations, if there is a need to test this function
- Deployment of Behavioral Health staff as deemed appropriate
PRE-INCIDENT INFORMATION
[One Month Pre Exercise]
- Your region has had an unusually wet season, with a record amount of rainfall. Extended rainfall has saturated the soil and caused runoff directly into streams and rivers, causing small area floods. Wet weather is expected to continue, and a slow-moving low-pressure storm system continues to produce heavy rainfall. Local street flooding has been continuous throughout the past month.
- The persistent rainfall has caused a [levee, dam, aqueduct, river, etc.] in your area to exceed the normal water elevation, and has been compromised. Officials have concerns that a failure could occur during future storms and this could result in a flash-flood scenario.
- Consider information regarding sand bag quantities, use, filling locations, delivery of sand bags, muscle walls, plastic sheeting, etc.
[One Week Before Exercise]
- During an intense and sudden rainstorm, flash flooding occurred on a [Main Local Highway]. Two vehicles were caught in the storm waters. One vehicle, a truck, was pushed off the road and the driver was rescued by local authorities. The other vehicle was pushed off the road and unfortunately was struck with debris and the driver was unable to exit the car and drowned.
- The [Local Health Department] and news stations are reminding the public with “Turn Around, Don’t Drown” messages.
- Flooding of a local recreation area has caused the mass relocation of a homeless camp. [Your jurisdiction] has had to establish a shelter for this newly displaced population.
- Local media is reporting widely on the storms headed to your area, and there are concerns that there may be additional flooding in the area.
- [Add any additional details relevant to your jurisdiction/agency/facility’s exercise]
EXERCISE INFORMATION
[Week of Exercise]
- The National Weather Service issues a [Flood Watch] for [Your jurisdiction]. The forecast calls for additional heavy rainfall, perhaps as much as 2-6 inches during the next 72 hours.
- The primary road used to access your facility is flooded and impassable.
- [Your facility, organization] has been contacted by the media to discuss the impact the road closure is having on your ability to provide services.
[Day before Exercise]
- As the storm continues, the National Weather Service issues a [Flash Flood Warning] for [Your jurisdiction]. It is estimated that flash flooding may occur within 12 hours.
- Areas around the [Agency, Facility] are experiencing minor flooding, including the parking lot and garage.
- The [local authority] has issued a voluntary evacuation for [insert County, City, Agency, Facility] and as a result, [Your facility, organization] is beginning to experience staffing problems. Road closures have affected the ability of some staff to report to work. Other staff are asking to return home.
- Many local schools and child care facilities are closing early today. Your [Agency, Facility] is experiencing staffing problems.
- Delivery drivers are unable to access your facility and you are not receiving critical shipments. Facilities on generator power may need extra fuel but delivery may not be plausible.
- [Add any additional details relevant to your jurisdiction/agency/facility’s exercise]
[Day of Exercise]
- The [local authority] has issued a [mandatory evacuation] for [insert County, City, Agency, Facility].
- Floodwaters reach your facility and cause significant damage on the first floor and supply storage areas.
- Large parts of [insert County, City] are without power, and some areas are without water.
- In some areas, residents have to be rescued from flooded homes and vehicles.
- Roadways remain flooded and impassable.
- Police officers have established a perimeter around heavily damaged areas, including your organization, and are not allowing anyone to enter for safety reasons.
- [Add any additional details relevant to your jurisdiction/agency/facility’s exercise]
ADDITIONAL NOTES
All Controllers and Evaluators are to note actual times and significant events on these MSELs and turn them into [Lead Evaluator] at the conclusion of the exercise.
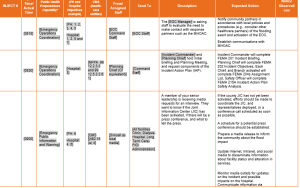

FLOOD SCENARIO HOSPITAL OBJECTIVES
How To Use This Document: The purpose of this document is to provide sample objectives
and capabilities for exercise planners to select from in designing their Statewide Medical and Health Exercise (SWMHE). These capabilities and their supporting objectives were identified based on the Multi-Year Training and Exercise Plan developed by the California Department of Public Health (CDPH). To access this document, please visit https://www.cdph.ca.gov/Programs/EPO/Pages/swmhe.aspx
To use this document, insert your agency/organization’s name in the bracketed text in the header that reads “INSERT NAME OF FACILITY/ORGANIZATION HERE.” Review the suggested capabilities and objectives and consider them as options to create an Exercise Plan that is customized to the unique characteristics of your organization and community. Select and modify as needed. According to the Federal Emergency Management Agency (FEMA), ten or fewer objectives are recommended for a functional exercise.
APPLICABLE CAPABILITIES
| Type | Capability | Capability Goal |
| HPP | Health Care and Medical Response Coordination | Health care organizations, the Health Care Coalition (HCC), and their jurisdictions collaborate to share and analyze information, manage resources, and coordinate strategies to deliver acute medical care to all populations during emergencies and planned events. Simultaneous response and recovery operations result in a return to normal or improved operations. |
| HPP | Continuity of Health Care Service Delivery | Health care organizations, with support from the HCC and the Emergency Support Function-8 (ESF-8) lead agency, provide uninterrupted, optimal medical care to all populations in the face of damaged or disabled health care infrastructure. Health care workers are well-trained, well-educated, and well-equipped to care for patients during emergencies. Simultaneous response and recovery result in a return to normal or, ideally, improved operations. |
| HPP | Medical Surge | Health care organizations – including hospitals, emergency medical services (EMS), and out of hospital providers – deliver timely and efficient care to their patients even when the demand for health care services exceeds available supply. The HCC coordinates information and all available resources for its members to maintain conventional surge response. When an emergency overwhelms the HCCs collective resources, the HCC facilitates the health care system’s transition to contingency and crisis surge response and its return to conventional standards of care. |
PROPOSED OBJECTIVES OBJECTIVE ONE
Alert and notify hospital staff of activation of the Emergency Operations Plan (EOP) and [insert other appropriate plans such as Flood or Utility Failure] within [insert time frame]. Health Care Preparedness and Response Capability 2: Health Care and Medical Response and Recovery Coordination
Sample Task(s):
- Utilize and test redundant communication systems [insert specific system to test, such as radio, email, mass notification software, etc.] to notify staff of the incident within [insert timeframe]
- Make appropriate notifications to staff (email, overhead page, etc.) and [insert facility/organization] within [insert timeframe]
OBJECTIVE TWO
Activate and staff the Hospital Command Center within [insert timeframe]. Health Care Preparedness and Response Capability 2: Health Care and Medical Response and Recovery Coordination
Sample Task(s):
- The Incident Commander will open the Hospital Command Center and activate the Hospital Incident Management Team (HIMT) down to the Chief level, and Section Chiefs will activate section personnel as needed within 30 minutes of initial incident notification
- Alert all staff of Hospital Command Center activation and relevant points of contact within the Hospital Command Center staff via [insert appropriate notification vehicle, such as email, text, or other internal notification system] within [insert timeframe]
- All personnel activated to HIMT positions locate associated Job Action Sheet, Hospital Incident Command System (HICS) Incident Response Guide, HICS 214 Activity Log, and HICS forms identified on the Job Action Sheet for their position
OBJECTIVE THREE
Develop an Incident Action Plan (IAP) within the first Operational Period for flood response. Minimum or HICS 201, 202, 204s and 215A or HICS IAP QuickStart form. Health Care Preparedness and Response Capability 2: Health Care and Medical Response and Recovery Coordination
Sample Task(s):
- Planning Section: gather situational information for Command and General Staff so that they may examine organizational ability to provide medical and behavioral health care based on the incident, and, as appropriate, provide information to staff and patients
- Operations Section: gather information on facility/facilities due to flooding for HICS 204
- Logistics Section: gather information on roadway and transportation impact from flooding for staff and patient transport for HICS 204
Finance Section: devise strategies to track all costs and expenditures of response, and estimate lost revenues due to canceled procedures, surgeries, and other services, and document this on HICS 204
- Report and document the incident by completing forms and submitting them to the Planning Chief within [insert timeframe] in each operational period:
- o Incident Commander: HICS 201 Incident Briefing – Establish Operational Period and work with Planning Chief on developing overarching objectives listed on the HICS 201 and 202, with Incident Commander giving final approval
- o Planning Chief: HICS 202 Incident Objectives
- o Section Chiefs and Branch Directors: HICS 204 Assignment List (for each Section/Branch activated)
- o Safety Officer: HICS 215A IAP Safety Analysis
- o Or utilize HICS IAP Quick Start
- Disseminate the approved IAP, to include the sharing of IAP information in incident briefings, to [insert other partners within your jurisdiction/agency/organization]
- Chiefs include Operational Period Objectives (from the 204 Assignment List form) for demobilization/recovery planning in each operational period
OBJECTIVE FOUR
Implement internal notification [insert strategies such as page, email, or intercom announcement] within [insert timeframe] for information and incident sharing within the hospital, between [XYZ Location, e.g., Labor Pool, HCC] and [XYZ Location, e.g., Triage Area, Pharmacy]. Health Care Preparedness and Response Capability 2: Health Care and Medical Response and Recovery Coordination
Sample Task(s):
- Utilize communications as an opportunity to update contact lists and directories in current facility EOPs and procedures (ensure contact data such as cell phone numbers is included, as most personnel are not at their office phone during emergency response). Compile and submit a list of updated contact information to the [e.g., Incident Commander] by the end of the exercise
- Complete and use [insert specific form/medium, e.g., HICS 213 General Message Form] to document all messages between the Infrastructure Branch and Operations Chief to share with the Hospital Command Center on facility status and impact of flooding
- Establish a secure radio channel and review proper radio etiquette within [insert timeframe] of Hospital Command Center activation with all those assigned a radio
- Public Information Officer (PIO): develop a message to patients about the situation with the flood and update Internet, Intranet, and social media to disseminate information about hospital status and alteration in services to patients, staff, families, and stakeholders
OBJECTIVE FIVE
Initiate communication strategies [such as page, email. etc.] within [insert timeframe] between Hospital Command Centers and the [the Medical Health Operational Area Coordinator (MHOAC), local operational area/Department Operations Center (DOC)/Emergency Operations Center (EOC)]. Health Care Preparedness and Response Capability 2: Health Care and Medical Response and Recovery Coordination
Sample Task(s):
- Issue, receive, and confirm incident information and message sent at least once to the MHOAC and message received at least once from the MHOAC
- Include at least one redundant system (e.g., satellite phones, radios, ReddiNet, WebEOC)
- Participate in the Joint Information Center (JIC), if established, through regular status updates, email, or an in-person designated representative. If flooding affects ability to travel to the JIC, use of virtual JIC can be exercised
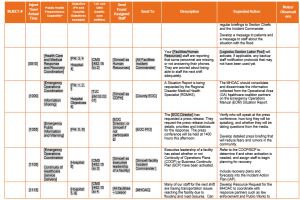
OBJECTIVE SIX
[Insert XYZ position, e.g., Medical Care Branch Director] will document the dispositions of victims through the continuum of care for the entire exercise timeframe, utilizing HICS 254 Disaster Victim Patient Tracking. Health Care Preparedness and Response Capability 2: Health Care and Medical Response and Recovery Coordination
Sample Task(s):
- Include on HICS 254 Disaster Victim Patient Tracking form the locations of victims/patients evacuated to alternative care sites or other areas if flooding affects existing treatment and patient bed areas
- Ensure that all Health Insurance Portability and Accountability Act (HIPAA) regulatory/confidentiality requirements are being met with all documentation used by assigning [insert an individual role] to review forms for compliance
- Track patients from entry into the healthcare system through discharge throughout the exercise
OBJECTIVE SEVEN
Assess and report hospital situation status, including flood damage to the facility, shelter-in-place or evacuation plans, on the HICS 251 Facility System Status Report and capability to provide care to Medical and Health Operational Area Coordinator (MHOAC) within [insert timeframe]. Health Care Preparedness and Response Capability 2: Health Care and Medical Response and Recovery Coordination
Sample Task(s):
- Provide information on the facility and bed status/bed capacity consistently on HICS 251 Facility System Status Report or applicable bed status sharing system, every [insert timeframe], to the [local operational area/DOC/EOC/MHOAC]
OBJECTIVE EIGHT
Activate and implement [e.g., Flood Plan or facility-specific plan including, evacuation, loss of utilities, HICS Incident Response Guides] within [insert timeframe] and deliver timely and efficient care. Health Care Preparedness and Response Capability 4: Medical Surge
Sample Task(s): Utility Failure, Shelter in Place
- Activate plans addressing Utility Failure, Flooding, Shelter-in-Place, and Evacuation that affect your current situation
- Examine current capability and develop additional strategies to increase and expand surge capacity as needed
- Identify resource constraints limiting surge capacity and describe strategies to increase resources within incident action plans and objectives
- Identify patients with access and/or functional needs and describe strategies to address those needs within IAPs and objectives
- Assess resource requirements during each operational period based on the evolving situation and coordinate with [insert relevant response partners] to obtain necessary resources during surge operations
- Address mitigation of potential losses (e.g., moving equipment and supplies)
OBJECTIVE NINE
[Insert specific position, e.g., Liaison Officer at the request of the Logistics Section Chief] to send at least one resource request through the Medical and Health Operational Area Coordinator (MHOAC) within [insert timeframe], and will communicate resource needs with Health Care Coalition partners to identify available assistance. Health Care Preparedness and Response Capability 2: Health Care and Medical Response and Recovery Coordination
Sample Task(s):
- Confirm communication and data interoperability for HCC partners
- Utilize appropriate resource request forms such as 213rr Resource Request (ensuring specific request, e.g., if requesting fuel for generators, specify fuel type and amount. For personnel, be specific on type, e.g., Pediatric Nurse, Registration, etc.)
- Activate plans and mutual aid agreements to obtain, share and/or return HCC resources as appropriate, going through the proper resource request and resource demobilization procedures [e.g., through the local Medical Alert Center (MAC) and/or MHOAC]
- Identify transportation issues for staff that require government intervention such as California Highway Patrol and coordinate with MHOAC
- Identify potential delivery issues for supplies due to road impacts and coordinate with MHOAC
- Identify transportation issues for patient transport and coordinate with MHOAC to ensure private and local EMS issues are addressed
- Review generator fuel need and potential needs, including transportation issues
OBJECTIVE TEN
Plan for the activation of mental and behavioral health services for all staff members and patients as part of incident response and recovery planning within [insert timeframe]. Health Care Preparedness and Response Capability 3: Continuity of Health Care Service Delivery
Sample Task(s):
- Coordinate with the MHOAC and local responding agencies to determine the need for additional behavioral and mental health services, partners, and volunteers to provide an appropriate level of care to staff, patients, and family members
- Coordinate with administration and leadership to facilitate access to and promote availability of mental and behavioral health services for staff, patients, and family members, including briefings for staff on educating patients and families on available resources
OBJECTIVE ELEVEN
Initiate collaborative efforts with the Infrastructure Branch and Medical Care Branch to identify mitigations for flood related staff and patient safety risks within [insert timeframe]. Health Care Preparedness and Response Capability 4: Medical Surge
Sample Task(s):
- Coordinate with Environmental Health to address the impact of contaminated flood waters
- Coordinate with local water districts to identify if local ground water is affected by the potential contaminated flood water through the Liaison Officer
- Coordinate with the Safety Officer, local public health, and environmental health to identify PPE needed for dealing with contaminated water
- Address any need for channeling water around facilities (e.g. sandbags, Muscle Wall, and plastic sheeting)
- https://www.cdph.ca.gov/Programs/EPO/Pages/swmhe_current.aspx ↵

