12 Chapter 12 Fatality management, Community Recovery, 101st WMD Civil Response Unit
Fatality Management
12.10 Discussion Forum on Fatality Management –Link to Canvas Site
For this discussion, you will be looking at the Fatality Management section of the textbook
Pre-Discussion Work
Read through the text book on Fatality Management. Then Select on of the 5 Functions within the document: for you discussion topic
• Function 1: Determine the public health agency role in fatality management
• Function 2: Identify and facilitate access to public health resources to support fatality management operations
• Function 3: Assist in the collection and dissemination of antemortem data
• Function 4: Support the provision of survivor mental/behavioral health services
• Function 5: Support fatality processing and storage operations
Drafting Your Response
Next, prepare your forum post by creating a document. On your document, answer the following questions:
- What interested you in the particular function?
- What is contained in the function that you did not expect to see listed?
- Thinking about the function you selected on a smaller scale say at an organization you work or have worked. How well do you believe that organization would do should they be involved in a mass fatality situation. Much like a van crash that kills an entire sports team or a plane crash that kills an entire executive team or key support group.
Be sure to support your responses by referencing materials from this module. Also, once you have answered the questions, be sure to proofread what you wrote before you share it.
Discussing Your Work
To discuss your findings, follow the steps below:
Step 01. After you have finished writing and proofreading your responses, click on the discussion board link below.
Step 02. In the Discussion Forum, create a new thread and title it using the following format: Yourname’s and the topic of the discussion board.
Step 03. In the Reply field of your post, copy and paste the text of your composition from the Document you created.
Step 04. Add bolding, underlining, or italics where necessary. Also, correct any spacing and other formatting issues. Make sure your post looks professional.
Step 05. If you need to upload a document or image you can do so by clicking on the Upload image (photo image button) or Upload document (Document button) in the text editor and locating and selecting your document from your computer.
Step 06. When you have completed proofreading, fixing your post formatting, and attaching your file, click on the Post Reply button.
Definition: Fatality management is the ability to coordinate with organizations and agencies to provide fatality management services. The public health agency role in fatality management activities may include supporting
• Recovery and preservation of remains
• Identification of the deceased
• Determination of cause and manner of death
• Release of remains to an authorized individual
• Provision of mental/behavioral health assistance for the grieving
The role may also include supporting activities for the identification, collection, documentation, retrieval, and transportation of human remains, personal effects, and evidence to the examination location or incident morgue.
Functions: This capability consists of the ability to perform the functions listed below.
• Function 1: Determine the public health agency role in fatality management
• Function 2: Identify and facilitate access to public health resources to support fatality management operations
• Function 3: Assist in the collection and dissemination of antemortem data
• Function 4: Support the provision of survivor mental/behavioral health services
• Function 5: Support fatality processing and storage operations
Summary of Changes: The updates align content with new national standards, updated science, and current public health priorities and strategies. Listed below are specific changes made to this capability.
• Clarifies importance of identifying the public health agency role in fatality management and describes potential fatality management lead, advisory, and support roles
• Aligns the fatality management definition to the existing federal definition as recommended by the
U.S. Department of Health and Human Services’ (HHS) Disaster Mortuary Operational Response Team (DMORT)
• Updates resources to improve coordination, accuracy, and timeliness of electronic mortality reporting
For the purposes of Capability 5, partners and stakeholders may include the following:
• emergency management agencies
• emergency medical services (EMS)
• federal authorities
• funeral homes
• funeral industry
• health care coalitions
• health care organizations
• hospitals
• law enforcement agencies
• medical examiner or coroner offices
• medicolegal authorities
• public health agencies
• subject matter experts (SMEs)1
• vital statistics partners
1 Including SMEs with expertise in epidemiology, laboratory, surveillance, community cultural or religious beliefs, or burial practices
Function 1: Determine the public health agency role in fatality management
Function Definition: Coordinate with jurisdictional authorities and partners to estimate and characterize potential fatalities and the impact of these fatalities on fatality management needs, resources, and activities to determine the public health agency role in fatality management.
Tasks
Task 1: Estimate fatality management needs based on jurisdictional risks . Characterize potential fatalities based on findings from jurisdictional risk assessment(s) and determine the resources and activities needed to manage potential fatalities based on the normal expected fatality rate and fatalities related to the incident.
Task 2: Clarify, document, and communicate the jurisdictional public health agency role(s) in fatality management . Coordinate with subject matter experts and cross-disciplinary partners and stakeholders to clarify, document, and communicate the public health agency role in fatality management based on jurisdictional risks, incident needs, and partner and stakeholder authorities.
Preparedness Resource Elements
P1: (Priority) Fatality management procedures that are scaled to address potential fatality scenarios based on jurisdictional hazards and risks. Jurisdictional fatality management procedures should be included in relevant jurisdictional emergency operation plans.
(See Capability 1: Community Preparedness)
P2: (Priority) Definition of the jurisdictional public health agency role for fatality management established in coordination with jurisdictional authorities, subject matter experts, and other cross- disciplinary stakeholders. Recommended activities to establish roles may include
• Identification of jurisdictional fatality management lead authority (individual or organization)
• Identification of public health liaison(s) to support fatality management operations and leadership
• Consideration of incident characteristics, existing plans, services, infrastructure, and information sharing needs in coordination with jurisdictional authorities and partners to determine public health support roles
· Incident characteristics
· Magnitude of incident, including the estimated number of decedents
· Condition of human remains (intact or fragmented human remains, meaning comingled, decomposed, charred, or mutilated)
· Rate of recovery (rapid, moderate, or slow)
· Recovery area complexity, including the extent of gridding necessary and whether recovery area boundaries are known or unknown
· Presence of hazards, including chemical, biological, radiological, environmental, or communicable disease hazards
· Disaster site location characteristics, such as fixed or distributed location and the need for excavation or debris removal
· Public health or law enforcement community constraints, such as limitations on public gatherings or establishment of curfews
• Event occurrence, such as single event at one location, single event at multiple locations, or recurring event at multiple locations
• Decedent identification needs, including antemortem data collection, postmortem data collection, requirement to issue death certificates, and communication with next of kin
· Existing plans, services, and infrastructure
· Medical examiner or coroner services and availability of interoperable case management system(s), mass fatality database(s), and electronic death registration system(s) (EDRS)
· Procedures to coordinate with other fatality management, funeral industry, and the American Red Cross to support investigations, relieve health care facilities, and support family, cultural, religious, and bereavement needs
· Death certification procedures to indicate that death is associated with a specific event, if applicable
· Public health laboratory plans for detection, characterization, confirmation, and reporting of public health threats based on testing of clinical specimens, food, water, and other environmental samples
· Health and safety plans for facilities and tasks involving hazardous work, such as complex recovery operations
· Plans to account for recovered remains and materials
· Family management services, including family assistance centers and long-term family management support
· Mental/behavioral services and grief or bereavement counseling for survivors, responders, next of kin, and affected communities
· Plans to coordinate with hospitals, health care facilities, and designated morgue facilities
· Information sharing needs
· Public messaging to identify human remains that should not be moved or manipulated
· Public messaging to communicate expectations for recovery, care, identification, and release of human remains
· Public messaging to communicate funeral capacity
· Information sharing with applicable jurisdictional committees, such as maternal mortality review or child fatality review committees
· Call centers to coordinate the collection of missing persons information and assist in prompt identification of remains
· Mortality reporting and information sharing requirements
· Press releases and social media announcements
· Death certificate record release to families
· Notification to the Federal Emergency Management Agency (FEMA), Veterans Affairs (VA), or other agencies and organizations to facilitate funeral or other benefits
P3: Written agreements, such as contracts or memoranda of understanding (MOUs) or co-signed plans among jurisdictional stakeholders that support coordinated fatality management activities to leverage shared resources, facilities, services, and other support based on identified roles.
P4: (Priority) Procedures in place to designate lead authorities to request resources based on ongoing assessments of the incident or event needs for example, public health agency response plans, coordinated with the jurisdictional emergency management agency, to facilitate state requests
for federal resources through HHS Regional Emergency Coordinators (RECs). Procedures for resource requests may include
• County or jurisdictional mass fatality protocols that indicate thresholds for requesting additional resources, including requests from local to state, state to state, and state to federal
• State, regional, and federal resources, including HHS DMORTs, to be requested when anticipated resource needs exceed local capacity
• Mutual aid agreements for resource requests, for example Emergency Management Assistance Compact (EMAC) or MOUs through appropriate channels, such as EMAC coordinator and emergency management
(See Capability 3: Emergency Operations Coordination and Capability 10: Medical Surge)
P5: Procedures in place, based on jurisdictional public health agency role(s), to support activities in coordination with partners and stakeholders.
(See Capability 1: Community Preparedness and Capability 13: Public Health Surveillance and Epidemiological Investigation)
Skills and Training Resource Elements
S/T1: Personnel trained on mass fatality or fatality management through courses offered nationally, by the state’s emergency management agency, the public health agency, or other partners, as applicable. Recommended trainings may include
• Center for Domestic Preparedness: Healthcare Leadership for Mass Casualty Incidents (MGT-901)
• Emergency Management Institute: Mass Fatalities Incident Response Course (G-386)
• FEMA Emergency Support Function #8—Public Health and Medical Services (IS-808)
• Rural Domestic Preparedness Consortium: Mass Fatalities Planning and Response for Rural Communities (AWR-232)
Equipment and Technology Resource Elements
E/T1: Personal protective equipment (PPE), such as protective clothing and respiratory equipment necessary to support fatality management procedures and activities.
(See Capability 14: Responder Safety and Health)
E/T2: Human remains pouches, facilities, and other equipment and locations to store human remains.
Function 2: Identify and facilitate access to public health resources to support fatality management operations
Function Definition: Develop recommendations to identify and facilitate access to resources, such as personnel and subject matter experts, record keeping, and physical space to address fatality management needs resulting from an incident in accordance with public health agency jurisdictional roles and standards outlined in jurisdictional fatality management procedures.
Tasks
Task 1: Assess incident data . Assess incident data to develop public health fatality management activity guidance and define resource needs.
Task 2: Develop and share incident-specific public health fatality management recommendations . Coordinate with jurisdictional, regional, private, and federal stakeholders as defined in the jurisdictional fatality management procedures to make incident-specific recommendations regarding the safe and efficient recovery, processing, reporting, storage, and final disposition of human remains.
Task 3: Initiate and coordinate public health support for fatality management operations .
Coordinate with identified stakeholders to operationalize strategies as defined in the jurisdictional fatality management procedures and share incident recommendations for managing human remains.
Preparedness Resource Elements
P1: (Priority) Procedures in place to collect and analyze incident data and develop recommendations for safe and efficient fatality management operations.
P2: (Priority) Procedures in place to identify and support public health agency lead or support activities for fatality incident management, including continuity of operations, based on incident data and recommendations. Public health agency activities for fatality incident operations, communication, and community support may include
• Mass fatality incident operations activities
· Coordinating with law enforcement and forensics agencies, such as medical examiners or coroners
· Participating in joint criminal-epidemiological (Crim-Epi) investigations
· Participating with the search and recovery of human remains
· Providing human health hazard mitigation and risk prevention and control recommendations
· Maintaining a roster of additional personnel
· Providing training on appropriate PPE
· Supporting security and preserving the mass fatality incident site
· Identifying multiple sites for interim storage and disposition of human remains
· Obtaining additional refrigerated space or equipment
· Managing the security and preservation of remains
· Implementing a tracking system for the identification of recovered remains
· Collecting and analyzing mass–fatality, incident-related mortality surveillance data
· Completing death certificates of decedents
• Communications and guidance activities
· Using communications systems to rapidly disseminate and receive incident health alerts
· Disseminating public communications, including the use of social media
· Providing guidance to the public on health and safety issues involving hazards and potential communicable disease(s)
· Providing guidance to the public on what to do if they find or know of the location of human remains, such as guidance to not move bodies from the scene
· Providing guidance on health and safety issues to prevent responder mortality
· Coordinating public affairs and establishing call centers
• Community resilience and support activities
· Organizing family assistance center(s)
· Facilitating the provision of funeral or other benefits for eligible next of kin from FEMA, VA, or other agencies and organizations
· Providing access to grief or bereavement and spiritual counseling
· Providing mental/behavioral health services to ease traumatic reactions experienced by responders and the public
(See Capability 4: Emergency Public Information and Warning, Capability 12: Public Health Laboratory Testing, Capability 13: Public Health Surveillance and Epidemiological Investigation, and Capability 15: Volunteer Management)
P3: Procedures in place to share information with fatality management partners, including fusion centers or comparable centers and agencies, emergency operations centers (EOCs), and epidemiologist(s), in order to provide and receive relevant intelligence information that may impact the response.
(See Capability 6: Information Sharing)
Skills and Training Resource Elements
S/T1: Personnel trained on functional activities based on designated jurisdictional fatality management roles.
Equipment and Technology Resource Elements
E/T1: Materiel to manage fatality operations based on the incident. Materiel may include
• Standard and hazardous materials (HazMat) PPE and clothing, such as gloves, boots, coats, hard hats, rain suits, and respirators
• Human remains pouches (appropriate number and type)
• Refrigerated storage
• Tents
• Equipment, supplies, and human remains storage
• Marking flags or barricade tape
• Barcoded toe tags
• Biohazard bags and boxes
• Photography equipment
• Gridding, laser survey, and global positioning systems
• Communication devices, such as radios and cell phones
• Equipment for scene documentation
• Hazard assessment or monitoring and mitigation unit
• Radiation survey equipment
• X-ray and laboratory equipment
E/T2: Data tracking systems that may be available through the medical examiner’s or coroner’s office to collect and manage data, which may include
• Missing person data
• Antemortem data, including DNA, medical or dental records, reported tattoos, and physical belongings
• Postmortem data, including human remains and scene data
(See Capability 6: Information Sharing)
E/T3: Death reporting systems available to ensure initial reporting (line lists) and accurate and timely completion of death certifications. Death reporting systems may include electronic mass fatality case management and incident systems, medical examiner or coroner case management systems, and electronic death registration systems.
Function 3: Assist in the collection and dissemination of antemortem data
Function Definition: Assist the jurisdictional fatality management lead authority and other partners including regional partners, as necessary, to gather and disseminate antemortem data through family assistance centers or other models, as defined in jurisdictional fatality management procedures.
Tasks
Task 1: Establish and refine antemortem data management processes . Coordinate with partners, such as family assistance centers to establish and refine processes and methods to collect and share antemortem data.
Task 2: Assemble necessary resources for antemortem data management . Coordinate with partners to support the identification and assembly of resources to collect and share antemortem data.
Task 3: Collect and share antemortem data with partners . Coordinate with partners to assist in the collection and dissemination of antemortem data to law enforcement, other agencies, and families of the deceased.
Task 4: Support electronic mortality reporting . Support recording and reporting of antemortem data through electronic systems or other information sharing platforms.
Preparedness Resource Elements
P1: (Priority) Procedures in place to collect and handle antemortem data in a secure and confidential manner, including data collection and dissemination methods, for example the use of call centers, family reception centers, and family assistance centers, and relevant personnel functions, such as interviews with families to acquire antemortem data, data entry, and administrative activities.
(See Capability 6: Information Sharing)
P2: Procedures in place for family notification, depending upon public health agency fatality management lead or support role(s). Procedures may include
• Contacting and notifying family members
• Releasing information in coordination with the medical examiner’s or coroner’s office
• Managing family expectations for decedent identification, such as fingerprint or DNA identification
• Handling and release of decedents’ personal effects
Skills and Training Resource Elements
S/T1: Personnel trained, as necessary, to assist in the collection and dissemination of antemortem data. Training may include
• Courses covering the following topics
· Providing relief to families after a mass fatality
· Supporting roles identified by lead agency
· Supporting family assistance and reception centers
• Courses offered by the National Transportation Safety Board (NTSB) Training Center, as necessary, which may include
· Family Assistance (TDA301)
· Advanced Skills in Disaster Family Assistance (TDA405)
· Emergency Accounting for Victims Following Transportation Mass Casualty Incidents (TDA406)
Equipment and Technology Resource Elements
E/T1: Central repository or database for the collection, recording, and storage of antemortem and postmortem data.
E/T2: Technology to establish call centers or toll free numbers to collect and disseminate information.
Function 4: Support the provision of survivor mental/behavioral health services
Function Definition: Support the provision of non-intrusive and culturally sensitive mental/behavioral health services to incident survivors, family members of the deceased, and responders according to the jurisdictional public health agency role for fatality management in coordination with the jurisdictional fatality management lead authority and stakeholders.
Tasks
Task 1: Assemble trained mental/behavioral health team(s) . Support the assembly of personnel and resources trained to provide mental/behavioral health services that are non-intrusive and culturally appropriate to accommodate the access and functional needs and religious or cultural practices of incident survivors, family members of the deceased, and responders.
Task 2: Support mental/behavioral health outreach services . Coordinate with stakeholders to support the provision of culturally appropriate mental/behavioral health services to incident survivors, family members of the deceased, and responders.
Preparedness Resource ElementsP1: (Priority) Procedures in place to identify, develop, and implement services for survivors, families, and responders in conjunction with jurisdictional mental/behavioral health partners. Procedures should reflect relevant cultural, religious, family, and burial practices.
(See Capability 1: Community Preparedness)
P2: (Priority) Pre-identified personnel and resources to provide mental/behavioral health services to survivors and families. Personnel may include
• Public and private agencies including specialized agencies for mental health, children, and aging, as appropriate to assist with the organization and provision of services
• Spiritual care providers
• Translators
• Embassy and consulate representatives, when international victims are involved
Skills and Training Resource Elements
S/T1: Personnel trained in mental/behavioral health-related fatality management activities, such as supporting family assistance centers.
S/T2: Personnel with cultural competency training as related to fatality management.
Function 5: Support fatality processing and storage operations
Function Definition: Support activities to ensure that human remains, associated personal effects, and official documentation are safely and accurately recovered, processed, transported, tracked, recorded including death certificates, stored, and disposed of or released to authorized person(s) according to the jurisdictional public health agency role and fatality management procedures.
Tasks
Task 1: Support the safe management of human remains . Provide health protection and safety guidance to incident management or the jurisdictional lead authority to ensure the safe recovery, receipt, identification, transportation, storage, and disposition of human remains.
Task 2: Support timely and accurate investigations . Support forensic and other investigations, as requested, to assist with the identification of hazards, risks, and cause and manner of death.
Task 3: Conduct death reporting . Coordinate with partners to support near-real time electronic death reporting during the fatality management incident.
Task 4: Ensure death recording in official documentation . Coordinate with partners to facilitate accurate and timely collection and recording of mortality information for official death certificates.
Preparedness Resource Elements
P1: (Priority) Procedures in place for the jurisdictional public health agency to coordinate with partners and stakeholders in fatality processing and storage operations, including procedures to monitor the location of human remains and storage capacity.
P2: Procedures in place for timely electronic death reporting in medical examiner or coroner case management systems or electronic death registration systems for information sharing. Recommended data elements for electronic death reporting may include
• Incident details, including date, time, location, and situation
• Victim identification, including name, date of birth, gender, ethnicity, height, weight, address, social security number, and medical history
- Victim relationships, such as identified family members and friends
- Location and types of injuries
- Cause of death (presumed, actual, or underlying)
- Death details, including date, time, location, and manner of death
- Circumstances that indicate whether the death was attributable to the event
- Human remains processing details
- Human remains storage location
- Health provider or responder details
- Survivor interview details
- Human remains disposition procedures
(See Capability 6: Information Sharing)
Skills and Training Resource Elements
S/T1: Medical examiners, morticians, and other relevant personnel trained to conduct their identified role.
Equipment and Technology Resource Elements
E/T1: Materiel and equipment to process, store, and release human remains for final disposition. Materiel and equipment may include
- Portable x-ray unit
- Morgue equipment, such as storage trailers
- Medical instruments for autopsies
- Radiation survey equipment
- Portable autoclave
- Gloves, gowns, and other PPE
- Digital cameras
- Specimen containers and preservatives
- Refrigerated storage
- Computers and printers
- Death certificate special embossed paper
Disaster Mortuary Operational Response Teams[1]
National Disaster Medical System
When natural or man-made disaster strikes, sometimes there are more fatalities than local resources can manage. Disaster Mortuary Operational Response Teams (DMORTs) support local mortuary services on location, working to quickly and accurately identify victims and reunite victims with their loved ones in a dignified, respectful manner.
DMORTs are deployed to supplement federal, state, local, tribal and territorial resources at the request of local authorities. On location during or after transportation accidents, natural disasters, terrorist attacks, and pandemics such as COVID-19, they focus on the recovery, decontamination, examination, identification, and return of deceased victims to help families, friends and communities find closure.
DMORT team members include
- Coroners
- Funeral directors/mortuary officers
- Medical examiners
- Forensic specialists (anthropologists, odontologists, pathologists)
- Dental assistants
- Autopsy assistants
- Fingerprint specialists
- Administrative specialists
- Logistics specialists
- Security specialists
- Safety specialists
- Diagnostic Radiologic Technologist
DMORT Capabilities
DMORT members provide technical assistance and consultation on fatality management and mortuary affairs. DMORTs may be called on to provide a wide range of services, including but not limited to:
- Tracking and documenting human remains and personal effects
- Establishing temporary morgue facilities
- Assisting in the determination of cause and manner of death
- Collecting ante-mortem data
- Collection of medical records, dental records, or DNA of victims from next of kin to assist in victim identification
- Performing postmortem data collection
- Documentation during field retrieval and morgue operations
- Performing forensic dental pathology and forensic anthropology methods
- Preparing, processing, and returning human remains and/or personal effects to appropriate recipients
- Processing and re-interment of disinterred remains
- Providing technical assistance and consultation on fatality management and mortuary affairs
Calling on NDMS [2]
The National Disaster Medical System (NDMS) supports state, local, tribal and territorial (SLTT) authorities following disasters and emergencies by supplementing health and medical systems and response capabilities. NDMS also supports its federal partners during National Security Special Events and it may be called on to support the military and Veterans Health Administration health care systems in caring for combat casualties, should requirements exceed their capacity.
The HHS Office of the Assistant Secretary for Preparedness and Response, in its role as Coordinator of Emergency Support Function 8 (ESF-8), Public Health and Medical Services, of the National Response Framework, employs the NDMS to provide patient care, patient movement, and definitive care, as well as veterinary services, and fatality management support when requested by authorities from States, localities, Tribes and Territories, or other federal departments.
NDMS is a federally coordinated health care system and partnership of the Departments of Health and Human Services, Homeland Security, Defense, and Veterans Affairs.
The mission of the Division of NDMS is to supplement our nation’s public health and medical resources, the Division of NDMS mobilizes resources through specialized teams that provide human and veterinary healthcare, mortuary assistance, patient movement coordination, and definitive care during times of need.
Getting Critical Support in a Crisis
NDMS teams provide many different types of public health and medical support to SLTT partners. NDMS personnel are required to maintain appropriate licensure and certifications within their discipline. When personnel are activated as Federal employees, licensure and certification is recognized by all States.
- Disaster Medical Assistance Teams
-
A Disaster Medical Assistance Team (DMAT) is a group of professional and para-professional medical personnel designed to provide medical care during public health emergencies or National Security Special Events (NSSEs).
Teams are capable of performing a wide range of patient-care functions in a variety of mission scenarios, including but not limited to:
- primary, acute, stabilizing emergency care
- emergency department decompression
- inpatient care augmentation
- supporting patient movement
- stabilization and transfer of all patients including ill/injured and nursing home patients
- staffing casualty/patient collection points
- triage services
- mass prophylaxis
- medical site/shelter operations
DMATs are a response resource that incorporates scalable deployment configuration sizes with specific clinical, non-clinical and leadership personnel. DMAT team members include advanced clinicians (nurse practitioners/physician assistants), medical officers, registered nurses, respiratory therapists, paramedics, pharmacists, safety specialists, logistical specialists, information technologists, communication and administrative specialists.
DMATs deploy to disaster sites with sufficient supplies and equipment to sustain themselves for a period of 72 hours while providing medical care at a fixed or temporary medical care site. The personnel are typically activated for a period of two weeks.
-
- Trauma and Critical Care Teams
-
The Trauma and Critical Care Teams (TCCT) are composed of medical professionals responsible for providing trauma and critical care support during public health emergencies and special events including National Security Special Events (NSSEs).
TCCTs can provide a deployable advance unit, augmentation to existing medical facilities, or establish a stand-alone field hospital. The capabilities of the TCCT include:
- critical care
- operative care
- emergency care
- advanced trauma life support
TCCT deployments often occur in austere environments. Personnel are deployed for fourteen day periods or longer and they leave when local medical resources are sufficiently recovered or have been supplemented by other organizations.
-
- Disaster Mortuary Operational Response Team
-
Disaster Mortuary Operational Response Team (DMORT) provide victim identification and mortuary services. DMORT provides expertise and support for:
- tracking and documenting of human remains and personal effects
- establishing temporary morgue facilities
- assisting in the determination of cause and manner of death
- collecting ante-mortem data
- collection of medical/dental records or DNA of victims from next of kin to assist in the forensic identification of the victims
- performing postmortem data collection
- documentation during field retrieval and morgue operations
- performing forensic dental pathology and forensic anthropology methods
- processing and re-interment of disinterred remains preparation
DMORT can also provide other technical assistance and consultation on fatality management and mortuary affairs as appropriate. Teams are composed of funeral directors, medical examiners, pathologists, forensic anthropologists, finger print specialists, forensic odonatologists, dental assistants, administrative specialist, and security specialist.
While DMORTs works under the delegated jurisdictional authority of the local or state Coroner or Medical Examiner, DMORT personnel, work under the overall command and control of the HHS Emergency Management Group (EMG) and/or the Incident Response Coordination Team (IRCT).
DMORTs may deploy with a Disaster Portable Morgue Unit (DPMU). The DPMU includes equipment and supplies for deployment to a disaster site. It contains a complete morgue with designated workstations for each processing element and prepackaged equipment and supplies.
-
- Victim Information Center Team
-
The Victim Information Center Team (VIC) is responsible for providing support to local authorities during a mass fatality or mass casualty incident by collecting ante-mortem data and serving as liaison to the victims’ families or other responsible parties in support of another NDMS team.
The VIC Team provides support by:
- collecting dental records, medical records, DNA, and other ante-mortem data
- providing subject matter expertise in mass fatalities management and victim information procurement
- training partners to appropriately gather the information required for victim identification from the family interview process
- explaining the HIPAA Privacy Rule Exemption for Medical Examiners and Coroners at 45 CFR 164.512(g)(1) to the medical and dental providers of the victims to facilitate obtaining these records
- coordinating and sharing data with morgue and forensic staff on a regular basis for potential identification
- coordinating with federal, state and local law enforcement agencies by gathering ante-mortem data to facilitate victim identification and manage the missing persons list
- updating the Victim Identification Program (VIP) database
- coordinating the release of remains
-
- National Veterinary Response Team
-
The National Veterinary Response Team (NVRT) is the primary Federal resource for the treatment of injured or ill animals affected by disasters. The NVRT is comprised of individuals with diverse expertise, including veterinarians, animal health technicians, epidemiologists, safety specialist, logisticians, communications specialists, and other support personnel. During a response, NVRT provides assessments, technical assistance, public health and veterinary services. Additionally, during a response, they are supported by a cache of equipment, supplies and pharmaceuticals.
NVRT members can provide support in the areas of veterinary medicine, public health and research. NVRTs can support SLTT partners by providing:
- assessments of the veterinary medical needs of animals and communities
- veterinary medical support to working animals which might include search and rescue dogs, horses, and animals used for law enforcement
- veterinary public health support including environmental and zoonotic disease assessment
- veterinary medical support to other deployed NDMS deployed teams
-
Community Recovery
12.11 Module 12 Worksheet-Idaho Rebounds–Link to Canvas Site
Directions: Download the worksheet12.11 Module 12 Worksheet-Idaho Rebounds
Begin by writing your name above. Then, using this sheet Your essay must address the following prompt:
- Review the definition of Community Recovery:
Community recovery is the ability of communities to identify critical assets, facilities, and other services within public health, emergency management, health care, human services, mental/behavioral health, and environmental health sectors that can guide and prioritize recovery operations. Communities should consider collaborating with jurisdictional partners and stakeholders to plan, advocate, facilitate, monitor, and implement the restoration of public health, health care, human services, mental/behavioral health, and environmental health sectors to at least a day-to-day level of functioning comparable to pre-incident levels and to improved levels, where possible.
Go to the Idaho Corona Virus Site
- Review the topics on the site i.e. Resources, Vaccine, Therapeutics, Behavioral Health, Providers, Testing, Long-Term Care, Governor’s Actions
- Respond to the following prompts:
- Based upon the definition how well do you believe Idaho has done in addressing community recovery? Explain your answer.
- Are there topics that you believe should have been added? Explain your answer.
- Select one of the topics and review the topic.
- Which topic did you select?
Do you believe that the material within the topic is adequate to address the recovery on Idaho. Why or why not
Definition: Community recovery is the ability of communities to identify critical assets, facilities, and other services within public health, emergency management, health care, human services, mental/behavioral health, and environmental health sectors that can guide and prioritize recovery operations. Communities should consider collaborating with jurisdictional partners and stakeholders to plan, advocate, facilitate, monitor, and implement the restoration of public health, health care, human services, mental/behavioral health, and environmental health sectors to at least a day-to-day level of functioning comparable to pre-incident levels and to improved levels, where possible.
Functions: This capability consists of the ability to perform the functions listed below.
• Function 1: Identify and monitor community recovery needs
• Function 2: Support recovery operations for public health and related systems for the community
• Function 3: Implement corrective actions to mitigate damage from future incidents
Summary of Changes: The updates align content with new national standards, updated science, and current public health priorities and strategies. Listed below are specific changes made to this capability.
• Highlights the need to define the jurisdictional public health agency recovery lead and support role
• Supports the National Disaster Recovery Framework (NDRF)
• Promotes integration of community partners to support community recovery and restoration
• Emphasizes engagement of community partners to access hard-to-reach populations to ensure inclusive communications that meet the needs of the whole community
For the purposes of Capability 2, partners and stakeholders may include the following: all parts of the whole community, such as individuals, businesses, nonprofits, community and faith-based organizations, and all levels of government.
Specific partners and stakeholders may include
• animal services and agencies
• childcare organizations
• chronic disease programs
• communicable disease programs
• community coalitions
• emergency management agencies
• emergency medical services (EMS)
• environmental health agencies
• fire and rescue departments
• groups representing and serving populations with access and functional needs
• health care coalitions
• health care organizations (private and community-based)
• health care systems and providers
• health care associated infection control programs
• housing and sheltering authorities
• human services providers
• immunization programs
• jurisdictional strategic advisory councils
• law enforcement
• media organizations
• mental/behavioral health providers
• public health preparedness programs
• schools and education agencies
• social services
• state office of aging or its equivalent
• surveillance programs
• volunteer organizations
Function 1: Identify and monitor community recovery needs
Function Definition: Assess the impact of an incident on the public health system in collaboration with jurisdictional partners and stakeholders to prioritize public health, emergency management, health care, mental/behavioral health, environmental health, and applicable human services recovery needs.
Tasks
Task 1: Identify jurisdictional community recovery priorities . Collaborate with jurisdictional partners and stakeholders to identify and document jurisdictional community recovery issues and priorities based on the impact of an incident on the population and critical assets, facilities, and other services within the public health, emergency management, health care, mental/behavioral health, and environmental health sectors.
Task 2: Identify the jurisdictional public health agency role in community recovery . In collaboration with the jurisdictional emergency management agency and organizations representing jurisdictional Emergency Support Functions (ESFs) and Recovery Support Functions (RSFs), identify the jurisdictional public health agency lead or support roles for community recovery.
Task 3: Identify recovery services to be provided by the jurisdictional public health agency, partners, and stakeholders . Determine public health agency, partners, and stakeholders services that can be provided for short- and long-term recovery operations, including previously identified services and new services, as appropriate, to address emerging community recovery needs.
Task 4: Solicit community input from jurisdictional partners and stakeholders . Request community input from jurisdictional partners and stakeholders regarding public health service recovery needs before and after the incident to understand recovery needs, issues, barriers, and trends.
Preparedness Resource Elements
P1: (Priority) Procedures in place for collaborating with jurisdictional partners and stakeholders to determine community recovery priorities and to define jurisdictional public health agency role(s) in community recovery. Considerations for determining community recovery priorities and the jurisdictional public health agency role(s) may include
• Recovery needs based on the scope of the incident and available assets, such as funding, volunteers, and other resources for responding to identified hazards
• Public health agency organizational structure, such as whether environmental health or mental/ behavioral health services are separate agencies, legal authorities, and existing jurisdictional public health agency mandates
• Short- and long-term public health service delivery priorities and recovery goals
• Periodic assessment of incident impact information to characterize the size or extent of the incident and the sectors and populations impacted
• Review, assessment, and organization of recovery needs to facilitate timely and efficient reporting to federal, regional, state, local, tribal, and territorial emergency management agencies to support situational awareness and resource requests
P2: (Priority) Procedures in place for how the jurisdictional public health agency and jurisdictional partners and stakeholders will assess, conduct, monitor, document, and follow up with public health, emergency management, health care, mental/behavioral and environmental health, and human services needs to support jurisdictional recovery efforts. Procedures may include conducting community assessments or mission scoping assessments (MSAs) performed by federal and state RSF personnel.
(See Capability 1: Community Preparedness, Capability 7: Mass Care, Capability 10: Medical Surge, and Capability 13: Public Health Surveillance and Epidemiological Investigation)
P3: Predefined procedures, egress (exit) strategies, staging locations, and community reception centers for addressing hazards if they persist in the community or environment over time.
P4: Procedures in place to identify state and applicable jurisdictional legal authorities that permit non- jurisdictional clinicians to be credentialed to work in emergency situations.
(See Capability 1: Community Preparedness, Capability 7: Mass Care, Capability 8: Medical Countermeasure Dispensing and Administration, and Capability 10: Medical Surge)
P5: Documentation of identified sectors and partners that can support short-, intermediate-, and long-term community recovery efforts, including services to address the access and functional needs of identified at-risk populations who may be disproportionately impacted by a public health incident or event.
P6: Regularly scheduled community sector forums or local emergency planning committee meetings for representatives from different community sectors to collaborate. Activities may include
• Developing continuity of operations (COOP) plans
• Coordinating overall jurisdictional public health continuity of operations and community recovery roles
• Establishing and maintaining organizational relationships
• Sharing promising practices or approaches to recovery from similar incidents
• Learning about jurisdictional response and recovery processes and policies
• Exchanging information to identify available recovery support services by sector, such as shelter, day care, spiritual guidance, animal care, food, medication support, and transportation
(See Capability 1: Community Preparedness)
Function 2: Support recovery operations for public health and related systems for the community
Function Definition: Facilitate collaboration among jurisdictional partners and stakeholders to build a network of support services to reduce adverse public health consequences resulting from the incident, and develop plans to expedite recovery operations as appropriate based on the jurisdictional public health agency lead or support roles.
Tasks
Task 1: Coordinate with jurisdictional partners and stakeholders to develop recovery solutions .
Identify courses of action to address persistent or emergent recovery issues and coordinate among health care, emergency management, education, nonprofit, and social services partners to design solutions, plans, and services based on jurisdictional public health agency lead or support roles.
Task 2: Educate the community about public health services . Coordinate with community partners and stakeholders from within and outside the jurisdiction to educate the community regarding recommended public health services through unified messaging.
Task 3: Notify the community of jurisdictional public health agency recovery plans . In coordination with other jurisdictional agencies, notify the community of jurisdictional public health agency recovery plans that support the restoration of public health, emergency management, health care, mental/behavioral health, and environmental health services during and after the acute phase of the incident.
Task 4: Notify the community of available public health services . In coordination with jurisdictional partners and stakeholders, communicate recovery services available to the community, with attention to the access and functional needs of populations that may be disproportionately impacted.
Task 5: Inform the community of disaster case management or community case management services . In collaboration with jurisdictional partners and stakeholders, notify the community of available disaster case management or community case management services for impacted community members.
Task 6: Coordinate with jurisdictional emergency management agencies to support mutual aid agreements with neighboring jurisdictions to provide recovery services . Partner with jurisdictional emergency management agencies when developing intra- and inter-state public health mutual aid and resource sharing agreements with neighboring jurisdictions for the provision of community recovery support resources and services.
Preparedness Resource Elements
P1: (Priority) Integrated recovery coordination plan that accounts for the jurisdictional public health agency lead or support roles. The integrated recovery coordination plan should include
• Major public health recovery priorities
• Short-, intermediate-, and long-term recovery issues based on known hazards
• Intended actions to address identified public health recovery priorities
• Expected or intended actions to support a federally-led recovery support strategy
P2: Procedures in place to routinely collect and share response and recovery information, including information about community recovery priorities resulting from cross-jurisdictional and inter-state coordination with organizations providing outreach to impacted populations. Procedures should specify who is responsible for developing messages and identifying audiences, such as community partners, the community at large, and populations disproportionately impacted by the incident.
(See Capability 4: Emergency Public Information and Warning, Capability 6: Information Sharing, Capability 8: Medical Countermeasure Dispensing and Administration, and Capability 11: Nonpharmaceutical Interventions)
P3: Procedures in place to support regular monitoring, surveillance, and reporting to track health, social services, and case management-related recovery over the long term, depending on the incident.
(See Capability 4: Emergency Public Information and Warning, Capability 6: Information Sharing, and Capability 13: Public Health Surveillance and Epidemiological Investigation)
P4: (Priority) Procedures in place within a stand-alone public health COOP plan or as a component of another plan to support community recovery. Procedures may include
• Definitions, identification, and prioritization of essential services needed to sustain public health agency mission and operations
• Procedures to sustain essential services regardless of the nature of the incident (all-hazards planning)
• Positions, skills, and personnel needed to continue essential services and functions (human capital management)
• Identification of public health agency and personnel roles and responsibilities in support of ESF #8— Public Health and Medical Services
• Scalable workforce reduction
• Limited access to facilities because of issues, such as structural safety or security concerns
• Broad-based implementation of social distancing policies
• Identification of agency vital records, such as legal documents, payroll, personnel assignments that must be preserved to support essential functions or for other reasons
• Alternate and virtual worksites
• Devolution of uninterruptible services for scaled down operations
• Reconstitution of uninterruptible services
• Cost of additional services to augment recovery
P5: Predefined statements (message templates) that address expected questions and concerns related to the incident. Public health spokespersons should consider strategies that may include
• Collaborating with jurisdictional partners and stakeholders to develop unified, timely, and consistent messaging across agencies
• Using message maps when interacting with jurisdictional media and community organizations
• Developing tailored messages, such as fact sheets to disseminate information to the public and responders to help amplify support for disaster survivors
(See Capability 1: Community Preparedness, Capability 3: Emergency Operations Coordination, and Capability 4: Emergency Public Information and Warning)
P6: Recovery strategies that guide the timely provision of public health, health care, and mental/ behavioral health care beyond initial life-sustaining care. Strategies based on the jurisdictional public health agency role may include
• Accessible, safe, and functional facilities to provide public health services, including restoration of facilities or designation of new facilities, as necessary
• Short- and long-term programs and services for disaster survivors, responders, and the public
• Programs and interventions for managing stress, grief, fear, panic, anxiety, and other medical, human services, and mental/behavioral health issues for disaster survivors, responders, and the public
(See Capability 1: Community Preparedness and Capability 14: Responder Safety and Health)
P7: Procedures in place to coordinate health and related community services for physical injury, illness, mental/behavioral trauma, or environmental exposures sustained as a result of the incident.
(See Capability 10: Medical Surge)
P8: Procedures in place to support environmental health operations.
(See Capability 11: Nonpharmaceutical Interventions, Capability 13: Public Health Surveillance and Epidemiological Investigation, and Capability 15: Volunteer Management)
Skills and Training Resource Elements
S/T1: Volunteers from the Medical Reserve Corps (MRC) and other sources, such as Emergency System for Advance Registration of Volunteer Health Professionals (ESAR-VHP) trained in expected roles and responsibilities for community recovery activities. Training programs may incorporate mental health or psychological first aid to address immediate post-disaster behavioral health needs.
(See Capability 15: Volunteer Management)
S/T2: Environmental health personnel trained in mitigation of public health hazards related to disaster debris removal, hazardous waste, radiation, sanitation, and vector control.
(See Capability 14: Responder Safety and Health)
Function 3: Implement corrective actions to mitigate damage from future incidents
Function Definition: Incorporate improvement observations from past incidents to inform actions needed to restore the public health, health care systems, mental/behavioral and environmental health, and human services sectors to at least a day-to-day level of functioning comparable to pre-incident and to improved levels, where possible. Document actions within written after-action reports (AARs) and improvement plans (IPs) and implement corrective actions based on jurisdictional public health lead or support roles.
Tasks
Task 1: Conduct post-incident assessment and planning for AARs and IPs . In collaboration with jurisdictional partners and stakeholders, conduct post-incident assessment and planning as part of the after-action process for short- and long-term recovery efforts.
Task 2: Facilitate collaboration between government and the community to develop corrective action plans . Facilitate and advocate for collaboration among government agencies and community partners to support the completion of agency-specific corrective actions.
Task 3: Collect community feedback for corrective actions . Collaborate with sector leaders to facilitate collection of community feedback to inform and identify corrective actions.
Task 4: Implement corrective actions into recovery plans and operations . Implement corrective actions that are within the scope or control of the jurisdictional public health agency for short- and long-term recovery, including the mitigation of damage from future incidents, in recovery plans.
Task 5: Develop a transition plan for implementing and monitoring corrective actions . In partnership with key stakeholders, create a transition plan based on the jurisdictional public health agency lead or support roles to integrate implementation and monitoring of corrective actions into day-to-day agency operations.
Task 6: Assess and strengthen community resilience to future disasters . Coordinate with jurisdictional partners and stakeholders to evaluate and strengthen community resilience to future incidents by improving routine community functioning and reducing community vulnerability. Based on the known or anticipated health and social services recovery issues
that the community will experience, integrate the necessary interventions for those issues and barriers into day-to-day business through inclusion in multiyear budgets, planning efforts, and staffing approaches.
Preparedness Resource Elements
P1: Procedures in place for continuous development and maintenance of partnerships with cross-sector community partners and stakeholders to support the restoration of access to public health, emergency management, health care, and mental/behavioral and environmental health services.
(See Capability 1: Community Preparedness)
P2: (Priority) Procedures in place to solicit feedback and recommendations from leaders in key sectors to improve community access to public health, emergency management, health care, mental/behavioral and environmental health, and human services. Key sectors may include
- Business
- Childcare
- Community and faith-based organizations
- Education
- Government
- Health care
- Housing and sheltering
- Media
P3: Corrective action plans based on jurisdictional public health agency lead or support roles that may include
- Mitigation plans to reduce damage from future incidents
- Jurisdictional and cross-sectoral models of community resilience to ensure the participation of all potential stakeholders in developing strategies to withstand and recover from future events
- Transition plan that identifies specific corrective actions, assigns them to responsible parties, and establishes targets for their completion
Disaster Recovery Plan Checklist[3]
Every disaster recovery plan must address, at a minimum, the following telecommunications items for the Provider Customer Service Program (PCSP). Each contractor shall identify the page(s) of their disaster recovery plans that pertain to each item. The contractors are not required to alter their existing disaster recovery plans, except to include each item, but may wish to create an overview document specific to PCSP telecommunications requirements.
• List of provider toll free numbers and what programs/services they support
• Current telecommunication configuration – where and how toll free numbers terminate
(i.e., into the switch, stand-alone IVR, VoIP, etc.).
• Location of critical equipment (i.e., ACD, IVR, PBX, etc.) and who is responsible for
maintaining the equipment. Back-up equipment should also be listed if applicable.
• Process for recovering, maintaining and restoring service for all contingency conditions
DISASTER RECOVERY CONDITIONS
- Short term outage (two days day or less)
- Long term outage (more than a two days)
- Loss of facility or inability to reach facility (plan to reconstitute at an alternate location)
• Percentage of CSR and IVR traffic (assuming normal conditions) that can be moved or managed under each disaster recovery condition. Each critical business function should also be addressed. For instance, plans might include call allocation plans, toll free number routing, and internal and external messages.
• Critical external contacts (i.e., telecom and data services service carriers, CMS, etc.) and who within your organization is responsible for contacting them.
• Emergency response teams with appropriate skills to carry out procedures for recovering, maintaining and restoring critical functions and processes.
• Critical internal contacts with a plan for information dissemination. Detailed information does not need to be included in the plan beyond the acknowledgment that such provisions are in place and ready to be executed.
Civil Support Teams – new tactics for new threats

By CW2 Marc Acton GX Magazine
ARLINGTON, Va. – After 9/11, the Department of Defense mandated that the National Guard increase its emphasis on the kinds of threats the United States was likely to see from terrorist organizations.
With the 9/11 attacks as a blueprint, terrorists’ new focus on weapons of mass destruction meant creating teams with more technology that would be able to respond to similar incidents around the country. One part of that effort to combat potential threats to our country’s safety was the creation of Weapons of Mass Destruction Civil Support Teams, or CSTs for short.
Congress authorized the first 10 teams in 1998. Due to the extensive training and operational tempo, the units are filled with Title 32, full-time Soldiers and Airmen. Today, one of these 22-man teams is in every state and the District of Columbia, plus Guam, Puerto Rico and the U.S. Virgin Islands, and two in California, New York and Florida.
Each of the 57 teams has to be ready to go anywhere in (or around) its state at any time, to address any number of threats. One of the ways they do this is by training regularly with local, state and federal response organizations. From the FBI to local law enforcement, CSTs build relationships with first responders and civilian authorities so when they’re needed, they’re prepared.
“The National Guard is postured all over the nation in little communities; we’re a community-based defense force,” says Maj. Gen. Timothy A. Reisch, adjutant general for the South Dakota National Guard, home of the 82nd CST. “The nature of the 82nd’s mission is to provide immediate response to local officials who are responding to an emergency.
“All disasters are ‘local,’ ” Reisch says. “The 82nd responds very early on to a local emergency or disaster and advises the local officials on exactly what they’re dealing with, does the analysis on the presence or absence of chemical agents, and then provides expertise on what types of response or dangers are present.”
That’s the CST mission in a nutshell. In a CBRN event, they figure out what is going on and then help civilian authorities understand how to fix it.
The Threats
The number of threats CSTs could face is endless. As our enemies conjure new and more unpredictable ways to harm us, CSTs across the country must be ready to respond to all of them. While the primary tool of terrorists will always be fear, the weapons they use can be anything from anthrax to radiological material in what’s referred to as a “dirty bomb.”
CST members don’t just respond to terrorist attacks. They’re also called to major disasters where normally safe chemicals are present. This makes familiarity with chemical threats crucial to mission readiness.
In terms of biological hazards, most people think of contaminants such as anthrax or ricin (a poison found naturally in castor beans) as the most common threats, which they are, but CSTs located in major transportation hubs like Hawaii’s 93rd CST are also aware of other dangerous biological contagions as a potential source of disaster.
According to Lt. Col. Lance Okamura, the 93rd unit commander, the Honolulu airport is especially vulnerable to potential biological breakouts because it’s such an international hub. “We are prepared to provide assistance for what I would call ‘nonbelligerent’ (or natural) biological threats,” Okamura says. “If there’s a potential breakout that comes through, we are fully prepared to provide support to incident commanders.”
When it comes to natural biological threats, it isn’t just Hollywood that sees viruses as a potential source of disaster. Governments worldwide spend billions of dollars planning and preparing for potential outbreaks of viruses like 2009’s swine flu. Contracting these viruses can be avoided just like any other communicable disease-practicing good hygiene, and, in the case of a large-scale outbreak, avoiding big gatherings of people.
As for man-made threats, the most recent major attack on U.S. soil came from the bombers at the Boston Marathon on April 15, 2013. After that, civilian authorities increased requests to CSTs to support major events. The 93rd supports events like the Ironman Championships and the NFL Pro Bowl, providing preventive monitoring and protection.
CSTs can identify hazards, assess consequences, advise on response measures, position themselves as a preventive measure, and assist with appropriate requests for additional support. The missions can range from identifying some kind of white powder to responding to an oil spill to protecting public figures at the State of the Union address.
“We don’t wait for things to happen,” 1st Sgt. Norman Peleholani from Hawaii’s 93rd says. “That’s what the civilians ask of us-to just be there, to have a presence, to be monitoring, and then if something happens, we’re already there.”[4]
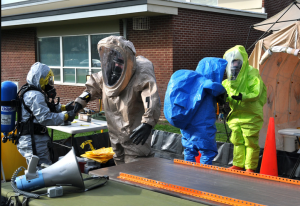
Mission: To support civil authorities at a domestic Chemical, Biological, Radiological and Nuclear high-yield Explosives (CBR- NE) incident site by identifying CBRNE agents/substances, assessing current or projected consequences, advising on response measures, and assisting with appropriate requests for additional follow-on state and federal military forces. Units can also provide immediate response for intentional and unintentional CBRN or hazardous material (HAZMAT) releases and natural or manmade disasters that result in, or could result in, catastrophic loss of life or property.
Overview: The Adjutant General may employ the Weapons of Mass Destruction Civil Support Team (WMD-CST) to support the state response under the direction of the governor or to support another state’s response under a supported governor. Each WMD-CST is comprised of 22 full-time, Title 32 Active/Guard/ Reserve (AGR), Army (ARNG) and Air National Guard
(ANG) personnel. The distribution of personnel on average is 18 ARNG and 4 ANG personnel, employed in 14 Army Military Occupational Skills or comparable Air Force Specialty Codes. The unit is divided into six sections: command, operations, communications, administration/logistics, medical/analytical, and survey.
A unit’s assigned transportation includes a command vehicle, operations trailer, a communications vehicle called the Unified Command Suite (which provides a broad spectrum of secure communications capabilities), an analytical laboratory system vehicle (containing a full suite of analysis equipment to support the complete characterization of an unknown hazard) and several general purpose vehicles. The WMD-CST normally deploys using its assigned vehicles, or can be airlifted as required.
A broad range of capabilities at a moment’s notice
 Highlights
Highlights
• Identify CBRN agents and substances, assess current and projected consequences, advise on response measures and assist with requests for additional support
• Operations mandated in statute
• Members receive more than 650 hours of HAZMAT and high-tech training from agencies such as the Federal Emergency Management Agency, the Department of Energy, the Department of Justice, and the Environmental Protection Agency
• Today, 57 WMD-CSTs are located in each state,
U.S. territory and Washington, D.C.; with two each in California, Florida, and New York
• On standby 24/7/365 days
• Advance team deploys within 90 minutes; the main body within three hours
• Operates a unique equipment set including a specialized/secure communications vehicle (Unified Command Suite), and a mobile analytical laboratory system with a full suite of chemical, biological, and radiological analysis equipment
WMD-CST Operations:• In FY15, there were 1,251 deployments for immediate response and stand-by support missions
• Units prepositioned to support the Boston Marathon, Super Bowl 49, papal visit, State of the Union Address, United Nations General Assembly, along with conducting numerous National and State Special Security Events and sports venues
Funding:• Federally resourced, trained, and sustained
• State controlled
- https://aspr.hhs.gov/NDMS/Pages/dmort.aspx ↵
- https://aspr.hhs.gov/NDMS/Pages/calling-ndms.aspx ↵
- https://www.hhs.gov/guidance/sites/default/files/hhs-guidance-documents/Disaster%20Recovery%20Plan%20Checklist.pdf ↵
- https://www.nationalguard.mil/News/Article/576636/civil-support-teams-new-tactics-for-new-threats/ ↵

