5 Module 05: Communication during an Emergency, Capability 4 Emergency Public Information, Warning and Capability 6 Information sharing, SOCO, Message Mapping
Public Information (PI)Introduction.
An act of biological terrorism is designed to generate significant amounts of public fear and apprehension that leave lasting impressions on victims and the population at large. The media’s goals are to monitor what’s happening around the community and to inform the public of any newsworthy occurrences. Any terrorist incident, be it biological, chemical, or explosive in nature, will be a major news story, as was seen in the September 11 World Trade Center (WTC) and Pentagon attacks. These types of stories result in a considerably strong public demand for accurate and timely information about the incident. It has been shown that public uncertainty and a lack of information will shape the public’s reaction and memory to a terrorist or disaster event. It seems self-evident that the media can play a significant role in shaping the public’s impressions of an event due to its role as the principal conduit of public information. The news media operates on a public mission in terms of purpose and franchise. This helps to distinguish journalism media from other forms of media expression. However, this distinction has become increasingly difficult to distinguish as the differences between the two have become blurred. Jurisdictions and community emergency planners need to look at ways in which various organization plans address the role of the media. Shortfalls in this area need to be addressed and exercised before an actual emergency.
Definition and Purpose.
Taken in the context of a bioterrorist incident, public information is information that the public uses to ensure safety within the community. It is information that people will use to make decisions and take actions that affect the protection of their lives, property, and the environment in which they live. Therefore, from an emergency management perspective, the purpose of public information and the media in particular is to convey key information to the affected community that will mitigate public panic, prepare the public for action, alert or warn the public, protect property, minimize environmental impact, save lives, and convince the public that the government has control of the situation (all of which were displayed during the days after the WTC and Pentagon attacks). Understanding these media functions and how each response organization has a vested responsibility to itself and the public may assist in the proactive planning collaboration.
Proactive Action.
It is essential to develop a plan to effectively utilize the media to educate the public and enhance the effectiveness of the response. Consideration needs to be given to developing communications strategies that bring the media into a partnership with consequence managers before the disaster. Bioterrorism plans and training exercises should be developed to anticipate and address public information issues that the community, the media, and emergency management agencies may face. Strategies should include a detailed plan for educating the public on what to do in such an event. This plan should be implemented during the mitigation phase of emergency response. The Internet or other routes of information dissemination will also be used to provide information to the public. The best chance of achieving the goals of mitigation and effective response is to enter into a partnership with the public during “normal” times. This effort may be greatly facilitated by the media via public information announcements. With-out adequate planning, reactive responses are normally ill-prepared or inaccurate, insensitive to the public’s needs/concerns, do not reduce fears or engender trust, and may leave the public with a negative feeling about the information that is released (i.e., the officials are hiding some-thing).
Rumor Control.
With many dead and many more sick, fear will set in quickly. There must be a consistent media campaign to get information to the public. Citizens must receive rapid information on where to go for treatment, where to locate loved ones, and how they are to respond when symptoms occur. Public health and safety information must be fully coordinated and issued “with one voice” so as not to confuse the public. This approach is equally important for the response community that must have accurate up-to-date information to deal with the public. The media can be a valuable asset if effectively brought on board. Ideally, the media will be given frequent information updates (as displayed by New York City’s Mayor Rudy Guiliani during the September 11 crisis) and have their questions answered as honestly and completely as possible. Blame assignment may begin very early. Any attempt to isolate the media would likely make things worse. Rumors increasingly fill the void left by the lack of information fl owing from the decision-makers. Such rumor generation may create excessive panic, fear, or civil unrest. Citizens will seek to understand what is occurring and what they need to do. Good information has a chance of helping citizens, while lack of good information is likely be a hindrance at best. The media is either going to be an ally in getting accurate information out or a foe by creating their own version of the events.
Obstacles.
Common misconceptions, misunderstandings, and the lack of information or knowledge can hinder the news media’s effectiveness in assisting emergency managers in handling the crisis. The following are challenges to an effective public information campaign.
1.Mutual Distrust. Perhaps the oldest obstacle is mutual distrust between response officials and the media. Typically, the media believes that government officials hide the truth, and the media must continuously search for the truth. Conversely, government officials may view the media as overly intrusive, sensationalizing the story or taking information out of context.
2.Availability of Information. Here two divergent approaches collide. Response officials want to be methodical in their analysis of the facts to ensure that they do not inaccurately identify the agent, provide incorrect response procedures, or mislabel the incident as a bioterrorist event. Inaccuracies could lead to public panic and jeopardize the public safety that they are trying to preserve and protect. Consequently, response officials typically release information only after careful deliberation. The news media is under tremendous pressure to continually provide information to the public. The deliberative approach used by response officials is not conducive to the media’s fast-paced requirements. As a result, if an “information vacuum” occurs, the media seeks other sources of information to fill the void. This makes frequent updates important (even if nothing has changed).
3. Lack of Knowledge of Health and Medical Issues. Some members of the media staff are specially trained to address various subject matter areas such as medicine and healthcare. This pool of individuals may be insufficient to cover the unfolding event. As a result, correspondents from other fields (e.g., legal, business, or national news) may be asked to cover the story. Their lack of familiarity with scientific or technical issues and jargon may result in unintentionally reporting incorrect or incomplete information.
4. For Profit Impact. The small family- owned newspaper and radio station is a relic of the past. Today large corporations have acquired most of the media operations and now press for a level of profit that is sometimes viewed as challenging honest reporting standards. Though most journalists, photojournalists and their support staff of engineers, producers, and editors are professional, conscientious, and accept their social and ethical responsibility to gather and report news fairly, accurately, and honestly, the influence of the large media corporations cannot be overlooked.
Potential Solutions.
There are three suggested approaches to overcoming the previously described obstacles. Each of these must be proactively initiated to be effective.
1. Training. Both media and responder community personnel need to receive training that is targeted to improve their interactions with one another. At a mini- mum, the lead emergency response officials should receive training to help them develop their skills in the following areas: community relations, media relations, writing, public speaking, and audio/visual presentation. These skills should be considered critical to the emergency management public information officer (PIO). This training would help minimize the potential for a spokesperson to be misunderstood or make ambiguous statements. Effective communications coupled with risk communications training is especially important in a bioterrorist incident where the need for clear and unambiguous information is paramount. The media should receive emergency response training designed to familiarize them in basic emergency response procedures that occur as a result of a bioterrorist incident. Improving the media’s awareness to timelines and normal response activities and the time required to conduct response activities can greatly aid in the development and accuracy of public information announcements.
2. Establishing Credible Experts and Accurate Information Sources. Credible Experts. The working group proposed that lead response officials identify credible experts to address media questions concerning a bioterrorist incident. As part of the emergency planning process, various bioterrorist agent or specific disease experts should be identified as part of the community or jurisdiction’s emergency response team. When a bioterrorist incident occurs, these individuals would be the recognized experts and the single point of information for the media. It is important to establish the presence and accessibility of credible experts before the information vacuum finds other potentially less credible or conflicting information sources.
Accurate Information Sources. Public attitudes and perceptions will be significantly affected by how a biological terrorism event is managed, and the quality and accuracy of the information that is provided. Accordingly, the relationship between emergency response management and the media is critical. The effect of uncontrolled and potentially distorted information could have disastrous effects on a stricken area. It is therefore critical to develop a dialog with responsible media personnel to examine ways in which credible options for information management and exchange can be secured. Incorporation of media planners into the emergency planning process could address these concerns up front and help to mitigate potential problems during an incident. Local, regional, national, and international media organizations may compete for the story. Technology has brought global events into our lives on a daily basis. News stories that are occurring throughout the world compete for the public’s attention and serve to dilute the focus away from other potentially more critical stories of local significance. This is true for emergency and disaster related stories that may initially go unnoticed due to other distractions. Pressures from competition could induce inaccurate media or emergency response reports. Public health and safety information officials, in partner- ship with media representatives, must maintain a “one voice of truth” that the public can trust. Misinformation will lead to public confusion, distrust, and potential non-compliance with incident- specific instructions and guidance.
3. Development of Bonds of Trust. Developing trust among the public, government/response officials, and the media is essential during times of public disaster and emergency. Bonds of trust are developed through routine personal interactions over time and are tied to historical performance (i.e., to what degree were you previously trustworthy?). Local officials and the media should take advantage of opportunities to interact with one another on a regular basis. This may be done in part by arranging understandings and agreements concerning emergency response operations in advance. Accuracy in reporting is vital for the public to trust the media. Reassuring the public and managing the crisis will be enhanced by a well-coordinated media plan. Despite establishing positive media relations, public health and emergency response officials anticipate that a bioterrorist incident may still cause widespread panic and fear.
Final Considerations
Good information is the foundation of a good policy. Addressing potential or real problems at the intersection of health and security must include efforts toward bolstering both the quality of and the transmission mechanisms for health-related information that may have security implications. Both sides of this issue have vested responsibilities, mutually to the public and their parent organization. Reporters will report more accurately if officials proactively offer information and assistance. Emergency managers who establish credible information
sources that are readily accessible are likely to find that the media will use these avenues for information gathering purposes rather than resorting to unsubstantiated “experts.” If there is a small release, public anger, not panic, will be directed toward the terrorist organization(s) but may also be directed towards any inadequacies perceived in law enforcement, fire protection, and public health response. Public health is a trust between the public and the government. The media, via public information, can be a bridge, keeping that trust intact. Ignoring or making assumptions about the media can be detrimental to that bridge. Public information/media are people with similar concerns and worries about an incident. Ameliorating panic can be achieved by showing that officials are in charge, have a game plan, are in control, know what they are doing, and are providing regular streams of up-to-date, valid and truthful information.
Editorial Note: During the remainder of this text book you will be seeing Capabilities that are listed from the
Public Health Emergency Preparedness and Response Capabilities: National Standards for State, Local, Tribal, and Territorial Public Health US Department of Health and Human Services Centers for Disease Control and Prevention.
This is the go to book developed by the Centers for Disease Control on responding to emergencies. Here is a direct link to the full documents.
Capability 4: Emergency Public Information and Warning
Definition: Emergency public information and warning is the ability to develop, coordinate, and disseminate information, alerts, warnings, and notifications to the public and incident management personnel.
Functions: This capability consists of the ability to perform the functions listed below.
• Function 1: Activate the emergency public information system
• Function 2: Determine the need for a Joint Information System
• Function 3: Establish and participate in information system operations
• Function 4: Establish avenues for public interaction and information exchange
• Function 5: Issue public information, alerts, warnings, and notifications
Summary of Changes: The updates align content with new national standards, updated science, and current public health priorities and strategies. Listed below are specific changes made to this capability.
• Promotes the need to leverage social media platforms for issuing emergency public information and warnings
• Clarifies conditions for establishing a virtual Joint Information Center (JIC) and Joint Information System (JIS)
• Includes content to identify and reach populations at risk to be disproportionately impacted by incidents and those with limited access to public information messages
For the purposes of Capability 4, partners and stakeholders may include the following:
• 911 authority
• community and faith-based organizations
• elected officials
• emergency management agencies
• emergency medical services (EMS)
• health care organizations• media organizations
• poison control centers
• public health agencies
• volunteer organizations
Function 1: Activate the emergency public information system
Function Definition: Notify and assemble key public information personnel and potential spokespersons identified prior to an incident to provide information to the public during an incident.
Tasks
Task 1: Identify key public information personnel . Identify public information officers (PIOs), spokespersons, and trained support personnel, such as subject matter experts to implement jurisdictional public information and communication strategies.
Task 2: Identify a primary and alternate physical or virtual JIC . Establish physical and virtual structures to support the creation and dissemination of health alerts and public information operations.
Task 3: Mobilize PIOs, spokespersons, and support personnel . Notify public information and communication teams of the need to be on call or report for duty within incident-appropriate time frames, including no-notice events.
Task 4: Establish roles and responsibilities of personnel to convey public information .
Assemble public information personnel at a physical location or virtually to establish roles and responsibilities.
Task 5: Ensure personnel are trained in the functions they may fulfill . Provide public information and communication education and training to PIOs, spokespersons, and support personnel according to jurisdictional need.
Task 6: Support local public health systems with the implementation of emergency communications . Clarify state, local, tribal, and territorial public health information roles and confirm communication support and coordination needs.
Preparedness Resource Elements
P1: (Priority) Procedures in place to document roles and responsibilities for PIOs, spokespersons, and support personnel based on the incident and subject matter expertise.
P2: (Priority) Message templates and risk communication message development to address identified jurisdictional risks and vulnerabilities related to incident characteristics. Recommended templates may include
• Stakeholder identification
• Potential stakeholder questions and concerns
• Key messages to address stakeholder questions and concerns
• Common sets of underlying concerns
P3: Primary and alternate physical locations or virtual structures to support the creation and dissemination of health alert and other emergency public information and warning operations. Personnel assembly can occur at a physical location, like an emergency operations center (EOC), virtual location, such as conference calls or web-based interfaces, like WebEOC, or combination of both physical and virtual locations.
(See Capability 3: Emergency Operations Coordination)
P4: Current roster or call-down lists with pre-identified personnel to participate in key emergency communications functions, including a minimum of one backup per role, as necessary.
P5: Procedures in place for personnel to notify and report for duty. Recommended notification procedures may include
• Notification methods, such as health alert network, e-mail, and other personnel notification methods
• Personnel notification time frame (how quickly personnel will be notified)
• Personnel reporting times and locations (may be virtual)
P6: Job action sheets that detail specific tasks for personnel and volunteer communications roles.
(See Capability 3: Emergency Operations Coordination and Capability 15: Volunteer Management)
P7: Systems and procedures to mobilize communication activities and roles applicable to the incident or event, such as information gathering, information dissemination, operations support, and liaison. One or more individuals may conduct activities and roles, which include
• Fact gathering
• Rumor control or message testing
• Monitoring and publishing content across print, Internet, social, and other media
• Providing support to speakers, such as developing talking points, speeches, and visuals
• Managing or responding to public inquiries using hotlines or other channels
(See Capability 3: Emergency Operations Coordination)
P8: Emergency communication implementation and coordination support to local public health systems from state and territorial jurisdictions.
(See Capability 6: Information Sharing)
Skills and Training Resource Elements
S/T1: (Priority) Public information personnel trained in relevant National Incident Management System (NIMS) courses, which may include
• Introduction to Incident Command System (IS-100.b)
• Incident Command System for Single Resources and Initial Action Incidents (IS-200.b)
• National Incident Management System, an Introduction (IS-700.a)
• National Incident Management System Public Information Systems (IS-702.a)
• National Response Framework, An Introduction (IS-800.b)
S/T2: (Priority) Public information personnel able to develop key messages using the principles of crisis and emergency risk communication. Within six months of hire and at least once every five years thereafter, the following trainings are recommended for completion
• CDC’s Crisis and Emergency Risk Communication (CERC) Basic Training
• CERC training administered by CDC personnel or local personnel already trained by CDC personnel
S/T3: PIO able to complete responsibilities, which may include
• Representing and advising the incident commander as part of the command personnel on all public information matters relating to communication management for the incident, and monitoring and handling media and public inquiries
• Managing day-to-day operations of the JIC and functioning within a JIS
• Coordinating with PIOs from participating government departments and organizations to manage resources and avoid duplication of efforts
Equipment and Technology Resource Elements
E/T1: Dedicated phone line(s) to receive and address inquiries from the media, stakeholders, and the public.
E/T2: Capacity for 24/7 health alerting (using phone or other alerting or notification methods), including maintenance, licensing, and mechanisms, such as contracts in place to purchase media time or short system messaging (SMS) code, as necessary.
E/T3: Redundant power supply to support 24/7 alerting and public messaging capacity.
E/T4: Communication devices to support partnerships with emergency management or other local authorities. Communication devices may include• Amateur radios
• Government Emergency Telecommunications Service (GETS) card issued by the U.S. Department of Homeland Security (DHS)
• Satellite phones
• Walkie-talkies, such as P25 compliant radios
• Other wireless devices
Function 2: Determine the need for a Joint Information System
Function Definition: Coordinate with emergency management agencies to determine the need for and scale of a JIS, including, if appropriate, activation of a new public health JIC. Participate with other jurisdictional JICs to combine information sharing abilities and coordinate messages.
Tasks
Task 1: Coordinate with jurisdictional emergency management to establish a public health JIC or a virtual JIC and participate in a JIS as needed . Activate a public health JIC or a virtual JIC, as applicable to the incident, and coordinate with emergency management to determine the need for a JIS.
Task 2: Ensure appropriate participation from public health communications representatives in the jurisdictional EOC . If a public health JIC is not activated for the incident, identify a public health communication representative, such as a PIO to participate in the jurisdictional EOC to ensure public health messaging capacity is represented.
Task 3: Coordinate public information messages through four common functions . Assign leads to the four common functions: information gathering, information dissemination, operations support, and liaison roles to public information personnel. Ensure coverage for extended operational periods, as applicable.
Preparedness Resource Elements
P1: Procedures in place to activate a JIC or virtual JIC connecting public information agencies or personnel through telephone, Internet, or other technologies and means of communication.
(See Capability 3: Emergency Operations Coordination)
P2: Standard operating procedures in place to request additional emergency public information and warning resources including personnel and equipment, and replace inoperable equipment to ensure continuity of operations through the jurisdictional incident management system.
P3: Decision support matrix to help determine when to scale up or scale down JIS operations. Recommended considerations may include
• Contingencies if incident information needs exceed the public health agen cy resources
• Procedures in place to detail how the public health agency will participate in the jurisdictional JIC or JIS if the response involves multiple organizations requiring coordinated messaging and spokespersons
Skills and Training Resource Elements
S/T1: Personnel or volunteers from partner agencies who will support information gathering, information dissemination, operations support, and liaison roles during an incident.
S/T2: Personnel or volunteers from partner agencies who have awareness-level training specific to media operations during an incident. Media operations may include television, Internet, radio, social media, newspapers, and other channels.
Equipment and Technology Resource Elements
E/T1: (Priority) Minimum components of a virtual JIC may include
• Electronic communications equipment to exchange information within the jurisdiction and with CDC in real time, as possible
• Plans for continuity of operations if equipment is inoperable
• Shared site, mechanism, or system to store electronic files of JIC products, e-mail distribution lists, incident information, and scheduling
E/T2: Supporting infrastructure for state, local, tribal, and territorial jurisdictions to send and receive information, with the ability to meet access and functional needs guidelines. Infrastructure may include
• Cellular phones
• Clocks
• Computers and printers
• Contact information for state and local officials and media
• Fax machines
• Internet access
• Phones and multiple phone lines
• Radio (dual-band, HAM, or high-frequency)
• Recording devices for both radio and television
• SMS text
• Television
• Video conferencing equipment
Function 3: Establish and participate in information system operations
Function Definition: Monitor jurisdictional media, conduct press briefings, and provide rumor control for media outlets using the principles of NIMS for organizing and coordinating incident-related communications.
Tasks
Task 1: Participate in public information sharing . Develop, recommend, and execute approved public health communication plans and strategies on behalf of the incident command or unified command structure based on the public health incident management role. Before sharing information with the public, collect, evaluate, and verify all information and obtain approval from authorized officials, such as health officer or incident commander.
Task 2: Control rumors . Control myths and rumors within the jurisdiction using media and digital outlets, including television, Internet, radio, social media, and newspapers.
Task 3: Provide a single point for dissemination of information for public health and health care issues . Release public health and health care information through pre-identified procedures based on jurisdictional processes, such as systems and spokespersons in coordination with the JIC.
Preparedness Resource Elements
P1: Procedures in place for when the public health agency may designate a lead PIO or provide public information support within emergency operations plans, job action sheets, or other applicable documentation.
P2: Procedures in place to track and monitor media, which may include
• Tracking media contacts and public inquiries, including contact, date, time, query, and outcome
• Monitoring media coverage to ensure information is accurately relayed
• Correcting misinformation before the next news cycle
• Addressing public health and health care concerns received from jurisdictional media interests
• Maintaining media contact lists and protocols for media engagement
Skills and Training Resource Elements
S1: Public information personnel trained in incident management and information systems operations. Relevant trainings may include
• National Incident Management System (IS-701.a)
• Emergency Management Institute G291—Joint Information System/Joint Information Center Planning for Tribal, State, and Local Planning Information Officers
• Emergency Management Institute PIO trainings
Equipment and Technology Resource Elements
E/T1: Equipment and digital media accounts that are accessible to PIOs or spokespersons in order to receive messaging from the jurisdiction’s public health alert system or network.
(See Capability 3: Emergency Operations Coordination or Capability 6: Information Sharing)
Function 4: Establish avenues for public interaction and information exchange
Function Definition: Provide methods for the public to contact the public health agency with questions and concerns. Methods may include
• Call centers
• Help desks
• Hotlines
• Instant messaging
• Social media
• Text messaging
• Websites
Tasks
Task 1: Establish systems for managing public and media inquiries . Implement scalable methods, such as Internet sites, call centers, poison control centers, non-emergency lines, such as 211 or 311, and social media to respond to public and media inquiries, as needed, for the incident.
Task 2: Post incident-related information on the public health agency website . Establish an Internet presence to inform and connect with the public that adheres to the principles of CERC.
Task 3: Use social media platforms and text messaging . Implement social media platforms, such as Twitter and Facebook and opt-in targeted notifications through texting, when and if possible, for public health messaging to the public.
Task 4: Identify, protect, and ensure information exchange with disproportionately impacted populations . Use geographic information systems (GIS), demographics, and epidemiological data to understand the complexities of the emergency and the response and to identify appropriate methods and sources, such as trusted spokespersons to protect, reach, and engage at-risk individuals with access and functional needs who may be disproportionately impacted by the incident.
Preparedness Resource Elements
P1: Procedures in place to activate and manage designated inquiry line(s), as applicable. Recommended procedures may include
• Diversion of unnecessary calls away from the community 911 system by establishing call centers or by other methods
• Diversion of non-critically ill patients away from the health care system, including the use of public information, advice, or triage lines
• Provision of updated public information regarding public health agency actions and recommendations
P2: Procedures in place to activate call centers with community partners, as needed. Recommended procedures may include
• Criteria for activating call centers
• Designation of persons to activate the call center system
• Designation of call center leader
• Process for call center system activation
• Procedures to detail how the call center will interface with the jurisdiction’s incident management system, to include the JIC
• Call center scripts or message maps for call center personnel
• Coordination of call center scripts with other messages
• Contact information for community partners for example, providing a public health center with poison control center contact information
• Processes to assess staffing needs
• Processes for staffing, increased hours, and demobilization of call centers
P3: Procedures in place for the usage of CDC-INFO or nurse triage lines and poison control centers as resources to increase response capacity for public and health care provider inquiries in emergency and natural disaster incidents, as applicable to the jurisdiction.(See Capability 6: Information Sharing)
P4: Procedures in place to monitor, manage, and use social media, which may include
• Addressing questions, myths, and misconceptions
• Collecting and reviewing digital media metrics, such as click-through rates, impressions, followers, likes, and shares
• Coordinating social media messaging with call center scripts
• Creating and clearing posts, including a time frame or schedule for adding new posts
• Evaluating social media engagement and reach
• Hyperlinking to other relevant websites
• Promoting social media channels
• Using geotags and push notifications to target social media messages to users in impacted areas
P5: Message development guidelines for social media, which may include
• Considerations for target audiences
• Use of plain language
• Character limits for messages
• Sign language interpreter and captioning for video messaging
• Audio conversion for scrolled messaging
• Actions the public can and should take during an incident
Skills and Training Resource Elements
S/T1: Public information personnel trained in the use of social media, technology, and health communication.
S/T2: Public information personnel who have completed NIMS Communications and Information Management training (IS-704).
Equipment and Technology Resource Elements
E/T1: Information technology or telephonic equipment to support the scalability of the inquiry line, as needed, for the incident (a transferred call occupies a phone channel until the call is completed).
Function Definition: Use CERC principles to disseminate critical health and safety information to alert the media, public, and other stakeholders to potential health risks and reduce the risk of exposure to ongoing and potential hazards.
Tasks
Task 1: Comply with jurisdictional legal guidelines when communicating information . Prevent communication of information that is protected for national security or law enforcement purposes or that may infringe on individual or entity rights.
Task 2: Disseminate information to the public using pre-established message maps . Disseminate approved messages to the public through multiple mechanisms, and ensure that languages and formats of information account for the access and functional needs of individuals, which may include individuals
- Who are deaf or hard of hearing
- With vision impairments
- With limited English proficiency
- From diverse cultural backgrounds
- With cognitive limitations
- Who do not use traditional media
Task 3: Disseminate information to responder organizations . Coordinate and transmit health- related information to responder organizations through secure messaging platforms.
Preparedness Resource Elements
P1: Documented and approved intra- and inter-jurisdictional legal authorities to avoid communicating information that is protected for national security or law enforcement purposes or that may infringe on individual or entity rights.
P2: Procedures in place to identify points of contact and establish a clearance process to verify and approve communication products, including talking points, social media messages, public information, and external-facing documents.
P3: Documented information to help populations at risk of being disproportionately impacted by an incident understand personal preparedness, what services are available, and where and how to obtain services. Consider the use of multiple media, multilingual materials, and alternative formats as well as the cultural appropriateness and age appropriateness of information.
P4: Procedures in place to address populations that may be disproportionately impacted by the incident, including at-risk populations with access and functional needs, in the development of informational materials.
P5: Procedures in place to reach rural or isolated populations.
Skills and Training Resource Elements
S/T1: Information technology personnel with necessary skills to support and sustain the jurisdictional health alert network or system.
(See Capability 6: Information Sharing)
S/T2: Personnel trained in health communication and cultural competency.[1]
Capability 6: Information Sharing
Definition: Information sharing is the ability to conduct multijurisdictional and multidisciplinary exchange of health-related information and situational awareness data among federal, state, local, tribal, and territorial levels of government and the private sector. This capability includes the routine sharing of information as well as issuing of public health alerts to all levels of government and the private sector in preparation for and in response to events or incidents of public health significance.
Function 1: Identify stakeholders that should be incorporated into information flow and define information sharing needs
Functions: This capability consists of the ability to perform the functions listed below.
• Function 1: Identify stakeholders that should be incorporated into information flow and define information sharing needs
• Function 2: Identify and develop guidance, standards, and systems for information exchange
• Function 3: Exchange information to determine a common operating picture
Summary of Changes: The updates align content with new national standards, updated science, and current public health priorities and strategies. Listed below are specific changes made to this capability.
• Increases alignment to public health surveillance and data strategies
• Emphasizes the need to implement data security and cybersecurity
• Emphasizes the need to decrease reporting time and increase collaboration by expanding use of electronic information systems, such as electronic death registration (EDR), electronic laboratory reporting (ELR), and syndromic surveillance systems)
For the purposes of Capability 6, partners and stakeholders may include the following:
• clinical and other professional organizations
• critical infrastructure services2
• emergency management agencies
• emergency response organizations3
• environmental health agencies
• federal, state, local, tribal, and territorial agencies
• food safety and agricultural representatives
• fusion centers
• hazardous material regulators and responders
• health care coalitions
• health care organizations
• health care providers
• health information exchanges
• immunization programs
• medical examiner or coroner offices
• mental/behavioral health agencies
• pharmacies
• private sector organizations
• public health agencies
• tribes and native-serving organizations
1 For example, water and electrical utilities
2 For example, law enforcement, fire departments, and emergency medical services (EMS)
Function 2: Identify and develop guidance, standards, and systems for information exchange.
Function Definition: Identify intra- and inter-jurisdictional stakeholders to participate in information exchange, and determine and periodically reassess stakeholders’ needs for bi-directional information sharing.
Tasks
Task 1: Identify intra- and inter-jurisdictional stakeholders to incorporate into information flow .
Identify intra- and inter-jurisdictional stakeholders to incorporate into information flow, and determine the information sharing needs for each stakeholder.
Task 2: Update and refine information sharing needs . Engage identified stakeholders regularly, and use quality improvement processes to continuously update and refine information sharing needs and capabilities.
Preparedness Resource Elements
P1: (Priority) Roster of identified stakeholders to engage for bi-directional information exchange across jurisdictional public health agencies and other partners and stakeholders.
P2: (Priority) Procedures in place to review and update the role-based public health directory that supports public health alert messaging. Recommended directory categories may include
• Organizational affiliation
• Assigned role(s) and notification tier
• Multiple sources of contact information, as available
(See Capability 4: Emergency Public Information and Warning)
P3: Established channels for stakeholder communications, such as standing meetings, electronic messaging, e-mailed communications, and web conferencing.
(See Capability 3: Emergency Operations Coordination and Capability 4: Emergency Public Information and Warning)
Equipment and Technology Resource Elements
E/T1: Information system(s) updated regularly and with appropriate backup to store and retrieve stakeholder contact information in a timely manner.
E/T2: System credentials and security clearances to access restricted information and systems, such as Epi-X, Homeland Security Information Network (HSIN), and the jurisdictional health alert network (HAN).
Function Definition: Define procedures and establish systems for information governance, management, and sharing.
Tasks
Task 1: Identify relevant data regulations, policies, and standards . Identify current jurisdictional and federal laws and policies that authorize, limit, or protect the exchange of information relevant to emergency situational awareness.
Task 2: Identify stakeholder data requirements . Coordinate with identified stakeholders to determine routine and incident-specific essential elements of information (EEI) for each stakeholder.
Task 3: Determine the conditions for information exchange . Identify when and to what extent information and data exchange is necessary for public health events and incidents.
Task 4: Develop systems for data storage and exchange . Identify and develop systems, such as electronic or non-electronic solutions to store, protect, control, and exchange data.
Task 5: Identify and mitigate barriers to information exchange . Use continuous quality improvement processes and corrective action systems to identify and mitigate procedural, legal, and policy-related barriers.
Preparedness Resource Elements
P1: (Priority) Procedures in place for information exchange that adhere to available national standards for health information exchange. Recommended standards and considerations may include
• Information exchange standards
· Security levels, such as sensitive, but unclassified or confidential
· Personnel authorized to share and receive information
· Timeline and frequency
· Data format, such as text or numeric and structure to ensure proper consumption in electronic health records (EHRs) and clinical decision support (CDS) systems
· Data use and release parameters
· Metadata needs
· Data privacy and cybersecurity
· Legal, statutory, and intellectual property regulations
• Other relevant considerations
· Inventory Data Exchange (IDE) dependent upon medical countermeasure type
· Electronic laboratory reporting (ELR), electronic case reporting (eCR), electronic death reporting (EDR), syndromic surveillance reporting, electronic laboratory test order and reporting (ETOR), immunization information systems (IIS), exchange of data among health jurisdictions, and data for other registries
· Environmental exposures data including hazardous material releases, air monitoring, water quality samples, food contamination, and radiation detection Monitoring of individuals in isolation or quarantine and monitoring of populations for contamination· Dissemination of clinical guidance for diagnostic evaluation and care
· Situational awareness briefings
(See Capability 9: Medical Materiel Management and Distribution and Capability 13: Public Health Surveillance and Epidemiological Investigation)
P2: (Priority) Stakeholder-specific procedures, determinants, trigger events or other applicable criteria for health information exchange. Determinants may include
• Epidemiology/Surveillance
· Unusual cluster(s) of illness that threaten closure of institutional settings, such as illness among health care workers or prisoners
· Large numbers of patients with similar and unusual symptoms
· Large number of unexplained deaths
· High burden of illness or a cluster of illness confined to a specific population
· Simultaneous clusters of similar illness in non contiguous areas for example, because of travel to affected areas
· Higher than expected morbidity and mortality associated with common symptoms or failure of patients to respond to traditional therapies
· Incidents in other jurisdictions that raise possible risk in an individual’s home jurisdiction including elevation of the pandemic influenza alert level
· World Health Organization’s (WHO’s) Public Health Emergency of International Concern (PHEIC)
· Laboratory
· Diagnosis or clinical, laboratory, environmental, or pathology finding of public health concern
· Public health laboratory findings not identified by clinical, surveillance, or epidemiological investigations, such as a novel virus
• Other
· Illness or injury burden expected to overwhelm local health care or public health resources
· Received threats or intelligence
· Mass casualty incident due to a catastrophic event, such as flood, earthquake, terrorism, or industrial release
(See Capability 10: Medical Surge, Capability 12: Public Health Laboratory Testing, and Capability 13: Public Health Surveillance and Epidemiological Investigation)
P3: Procedures in place for data exchange in both routine and incident-specific settings, including agreed upon systems for data storage and exchange and data exchange frequency with CDC and other stakeholders, in accordance with jurisdictional standards.
P4: Strategies for collaboration and system integration to improve intra- and inter-jurisdictional information sharing for situational awareness during routine operations and public health events or incidents. Consider collaborative strategies and activities, which may include
• Increasing information system interoperability to support disease and syndromic surveillance, public health registries, outbreak management, exposure assessment, and other activities
• Extending data availability with dashboards and other information sharing tools
P5: (Priority) Written agreements, such as contracts or memoranda of understanding (MOUs) with relevant agencies and other stakeholders to define participation, security or access levels, and procedures for information exchange.P6: (Priority) Procedures in place to account for laws, provisions, and policies addressing privacy, security including cybersecurity, civil liberties, intellectual property, information sharing limitations, and other substantive issues. Relevant laws and policies may include
• Emergency powers for public health data collection and sharing
• Health Insurance Portability and Accountability Act (HIPAA)
• Office of the National Coordinator for Health Information Technology Policy
• U.S. Department of Health and Human Services (HHS) Information Management Policy
• State laws and regulations prohibiting information sharing to federal or inter-jurisdictional entities
P7: Guidelines for information exchange that requires security clearances, such as information exchange with the Federal Bureau of Investigation (FBI), state bureau of investigation, fusion centers, or agents with a “need to know.”
Skills and Training Resource Elements
S/T1: Personnel with awareness-level training in pertinent laws and policies for information sharing procedures including transport of data and use of personally identifiable information (PII).
S/T2: Personnel trained in informatics and information technology project management, as necessary, to implement public health informatics systems.
Equipment and Technology Resource Elements
E/T1: Information systems that meet national data standards for interoperability as identified by CDC, other federal agencies, such as the Office of the National Coordinator for Health Information Technology, or other standards development organizations (SDOs). Recommended information system capabilities may include
• Receiving and transmitting data electronically using standards-based messaging
• Converting non-standard formats or terminologies into federally accepted standards for communication
• Receiving, using, and transmitting messages that adhere to certified EHR technologies or standards under Meaningful Use guidelines
• Transmitting and receiving data from non-electronic data sources, only if electronic capabilities are unavailable
• Gathering EEI or data from cross-disciplinary stakeholders and transmitting data into a public health situational awareness system
Function 3: Exchange information to determine a common operating picture
Function Definition: Share information across public health agencies and intra- and inter-jurisdictional stakeholders using available national standards, such as data vocabulary, storage, transport, security, and accessibility standards.
Tasks
Task 1: Exchange health information . Exchange meaning request, send, and receive relevant data and information with identified cross-disciplinary stakeholders using procedures and systems that meet jurisdictional or federal standards.
Task 2: Maintain accessible data repositories . Support information exchange among cross-disciplinary stakeholders using accessible data repositories that adhere to jurisdictional or federal standards.
Task 3: Apply data security protocols . Request, send, and receive information using security protocols that meet jurisdictional or federal standards.
Task 4: Verify data authenticity . Confirm data authenticity with message sender or information requestor.
Task 5: Acknowledge receipt of information . Confirm the successful transmission and receipt of information, as appropriate, for the incident.
Preparedness Resource Elements
P1: (Priority) Procedures in place to develop information and public health alert messages. Procedures may include
• Time sensitivity of information
• Relevance to public health
• Target audience
• Security level or sensitivity of information
• Actions required following the receipt of information, such as sending a response
(See Capability 4: Emergency Public Information and Warning)
P2: (Priority) Procedures in place for information exchange with fusion centers and other intelligence entities. Procedures may include
• Defined intelligence requirements that prioritize and guide planning, collection, analysis, and information dissemination efforts
• Delineated roles, responsibilities, and requirements for each level and sector of government
P3: (Priority) Procedures in place for information exchange among jurisdictional health care entities using electronic public health case-reporting systems, syndromic surveillance systems, notifiable disease surveillance systems, electronic death registration systems, immunization information systems, or other specialized registries. Data should be shared using electronic systems when available or as possible.
Electronic information sharing may include
• Sharing reportable diagnoses and related information from a health information exchange (HIE) or an EHR system to state and local public health agencies
• Sharing laboratory test results from commercial, public health, hospital, and other laboratories’ laboratory information management system (LIMS) to state and local public health agencies• Sharing laboratory test orders and results between a public health laboratory and another laboratory or a clinical setting
• Sharing immunization information between an HIE or EHR system and public health immunization registries, public health syndromic surveillance systems, such as CDC’s National Syndromic Surveillance Program BioSense Platform, or other public health registries
• Sharing notifiable disease data among public health agencies and between public health agencies and CDC
• Sharing information regarding individuals undergoing health monitoring or in isolation and quarantine
P4: Procedures in place to acknowledge receipt by trusted sources and send verification of information to intended audience(s).
P5: Templates for public health alert messages and procedures including distribution methods to ensure messages reach intended individuals 24/7 year-round. Public health alert message templates may include
• Subject or title
• Description
• Background
• Request or recommendations (if action requested)
• Recipient(s)
• Point of contact to address additional questions
• Links to additional information
(See Capability 4: Emergency Public Information and Warning)
P6: Information Sharing and Access Agreements (ISAA) or similar agreements with data sharing partners. Recommended elements for ISAAs may include
• Breach notification procedures, particularly if data is not stored in an encrypted state
• Maintenance of HIPAA Security Rule compliance, when potential PII must be shared
Skills and Training Resource Elements
S/T1: Personnel, such as informaticians trained on public health information systems to develop, sustain, coordinate, and oversee public health informatics.
S/T2: Information system support personnel trained, as necessary, to maintain or enhance the functionality and capacity of public health information systems, perform public health information specialist and informatics roles, and use data standards and facilitate interoperability across allied disciplines, including the Open Geospatial Consortium.
Equipment and Technology Resource Elements
E/T1: (Priority) Electronic systems for routine information transmission, emergency notification, and situational awareness between health care and public health systems and between jurisdiction-based surveillance systems and CDC that meet applicable national and jurisdictional standards. Standards may include
- Data format and structure
- System interoperability
- Data quality and reliability
- Consent, security, and privacy for protected health information and other sensitive information, as applicable, such as protections against data breaches using encryption
- Data governance or ownership and rules or agreements for data use, reuse, release, and publication
- Controls and safeguards for data storage and access that may include
- Authentication service for data requests and submissions from various locations
- System administrator password policies
- Updated security patches
- Encryption, as required
(See Capability 3: Emergency Operations Coordination and Capability 13: Public Health Surveillance and Epidemiological Investigation)
E/T2: Systems that automate transmission of information from the clinical setting, such as an EHR system, to the public health agency in compliance with jurisdiction-specific reporting regulations to support overall public health surveillance, improve the timeliness and accuracy of data submitted to state and local public health agencies, and enable subsequent information sharing with CDC.
E/T3: (Priority) Secondary systems for information sharing and public health alerting in the event that the primary system is unavailable.
(See Capability 4: Emergency Public Information and Warning)
E/T4: Data visualization tools, such as analytic dashboards and geographic information systems (GIS) for effective presentation and dissemination of data for situational awareness in routine and response situations.
Tools for Communication
There are multiple tools used for communication during a time of emergency. The two presented here are the Single Overriding Communication Objective and the concept of Message Mapping.
Single Overriding Communication Objective
This is a tool that allows you to organize your thoughts around a specific topic and actually allows you to get ready for a press interview. This is a handy tool to have in your desk and when an incident occurs that might impact your organization one can quickly jot down some thoughts and be ready should you be asked about the topic. If there is a public health situation in another part of the country the press often would like to get “local flavor” and may come to you to ask what your health facility is doing about such a situation in the local community.
05.05 Module 05 Discussion Forum – Developing a Single Overriding Communication Objective – Link to Canvas Site
For this discussion, you will develop a Single Overriding Communication Objective (SOCO) for an outbreak of measles that is occurring in your community. This is in preparation for a press release that you will develop for the second Discussion in this module.
Pre-Discussion Work
To begin this assignment, review the video on developing a SOCO.
Review information from the CDC on measles:
Signs and Symptoms of measles (Links to an external site.)
Transmission of measles (Links to an external site.)
Vaccination for Measles (Links to an external site.)
Situation in your community
The following in the situation in your community that you will need to develop your SOCO for and ultimately your press release.
A teenager with measles was infectious when she visited Roaring Springs, The Eight Street Market Place and other heavily visited sites in Southern Idaho earlier this month, public health officials said.
The teen was on a trip from Upper Slabovia and flew into the Boise Airport. The person visited Roaring Springs and Wahoos, among other attractions from Aug. 11 to Aug. 15. The person also reportedly traveled to The Village Shopping Center, Albertson’s Market Place Grocery Store and the Eagle Island State Park Swimming area during the trip,
Drafting Your Response
Next, prepare your forum post by creating a Google document. On your document, respond to the following prompt:
- Using the resources develop your SOCO for this incident.
Be sure to support your responses by referencing materials from this module. Also, once you have answered the questions, be sure to proofread what you wrote before you share it.
Discussing Your Work
To discuss your findings, follow the steps below:
Step 01. After you have finished writing and proofreading your responses, click on the discussion board link below.
Step 02. In the Discussion Forum, create a new thread and title it using the following format: Yourname and the topic of the discussion board.
Step 03. In the Reply field of your post, copy and paste the text of your composition from the Document you created.
Step 04. Add bolding, underlining, or italics where necessary. Also, correct any spacing and other formatting issues. Make sure your post looks professional.
Step 05. If you need to upload a document or image you can do so by clicking on the Upload image (photo image button) or Upload document (Document button) in the text editor and locating and selecting your document from your computer.
Step 06. When you have completed proofreading, fixing your post formatting, and attaching your file, click on the Post Reply button.
Below is the general outline of how you develop a SOCO.
PURPOSE Of SOCO
Advisories need a clear, consistent message. The SOCO (Single Overriding Communication Objective) Worksheet is a tool to create a specific message. Use the message developed in the SOCO Worksheet for all communication with the public and partners, including briefings and press releases. The point of contact information identifies the communication contact for the advisory. The SOCO approach applies to any communication.
DIRECTIONS
Work with staff and partners to complete the SOCO Worksheet. Use the best available information. First, think about the reason for the concern and the actions needed. Next, answer each question. Use the results to develop all communication. As the situation changes, use this worksheet to update the message.
……………………………………………………………………………………………………………………………………………………………………
Key Message: Provides Meaning and Context
In one brief paragraph, state the key point or objective you want to communicate.
Key Facts
What are the three most important facts you need an individual to understand about the public health situation?
- Key Fact
- Key Fact
- Key Fact
Target Audience
Who is the main audience or population segment you would like this message to reach? Who is the secondary audience? Finally Who would be next level of audience
Primary Audience:
Secondary Audience:
Tertiary Audience:
Communication Objective
What is the one message or action someone needs to understand?
Primary Contact
Who in your office/organization is the primary point of contact?
Name: ____________________________________________________________________________________
Phone: ____________________________________________________________________________________
Date and time available: ______________________________________________________________________[2]
Social Media Postings
The use and impact of social media platforms (e.g., Twitter, Facebook, LinkedIn, Snapchat, Instagram, TikTok, and YouTube) has skyrocketed over the past decade and has significantly supplemented—if not nearly replaced—more traditional means of communication for many population groups in the U.S. There are four primary ways that healthcare, public health, and emergency management use social media: posting information for public knowledge, posting to correct misinformation or rumors, obtaining incident information to help allocate resources, and identifying questions and issues to be addressed.
Recent disasters and mass casualty incidents have highlighted the level to which victims, family members, and responders use social media to communicate about issues such as: their status and location, the effect of the disaster on their surroundings, where and how to locate shelter and supplies, how to volunteer, and health and medical advice.
In addition to building community relationships and emphasizing preparedness and resilience pre-disaster, planners can use social media to identify and monitor potential threats to public health, and communicate with residents about threats (e.g., infectious disease), pending incidents (e.g., severe weather), and the location and availability of services (e.g., shelters and points of distribution). Tools such as crowdsourcing (collecting information from a large group of people via the Internet) and data mining bolster these efforts. Photos and live-streamed video can help amplify messaging, provide locational data, and communicate the urgency of a situation. [3]
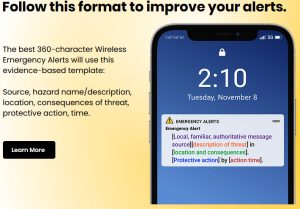
The following photo shows the suggested format for a social media post.[4]
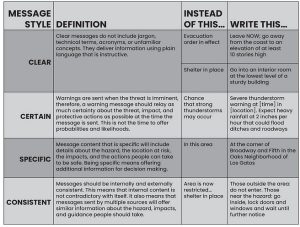
When developing the various aspects of the message one needs to pay attention to the Content and Style. The following graphics show how each is to be developed.
Content Guide:
Effective warnings are supported by decades of empirical research. Social scientists have identified message contents and message style that affect protective action decision making among those at risk. By including these contents, you can increase the likelihood that a person who is at risk will take action and decrease their protective action delay.

[5]
Style Guide
The style in which message content is relayed can be just as important as the contents that are included. Below is a short list of how to improve the style of a warning message. Use the definitions as SEARCH terms to see examples of these types of messages in the blogs.
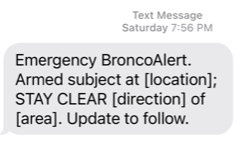
Every one at Boise State University that is on campus is encourage to subscribe to BroncoAlert. This is an example of an alert that was sent out with proof reading it. They have the format for the alert but someone forgot to fill in the blanks. This is an example of having your messages ready to go and not having to make them up on the fly. One just hopes that the blanks get filled in by the person on duty.
Message Mapping
05.08 Assignment Module -Developing a Message Map-Link to Canvas Site
For this assignment you will first of all develop 5 possible questions that may be asked during the interview. You will then take one of the questions and develop a message map on the form below.
Download the worksheet with the message map template 05.08 Assignment Module 05 – Developing a Message Map.docx
This is the first time you have done something like this so do not stress out about it. Give it you best effort. Developing a message map is extremely complex and is usually done with a team of people. The purpose of this exercise it to give you practice using the tool.

This is a photo of polio ward with iron lungs to help the patients breath.
In the late 1940s, polio outbreaks in the U.S. increased in frequency and size, disabling an average of more than 35,000 people each year. Parents were frightened to let their children go outside, especially in the summer when the virus seemed to peak. Travel and commerce between affected cities were sometimes restricted. Public health officials-imposed quarantines (used to separate and restrict the movement of well people who may have been exposed to a contagious disease to see if they become ill) on homes and towns where polio cases were diagnosed.
Polio was once one of the most feared diseases in the U.S. In the early 1950s, before polio vaccines were available, polio outbreaks caused more than 15,000 cases of paralysis each year. Following introduction of vaccines—specifically, trivalent inactivated polio virus vaccine (IPV) in 1955 and trivalent oral poliovirus vaccine (OPV) in 1963—the number of polio cases fell rapidly to less than 100 in the 1960s and fewer than 10 in the 1970s.
Thanks to the polio vaccine, dedicated health care professionals, and parents who vaccinate their children on schedule, wild poliovirus has been eliminated in this country for more than 30 years.
- Since 1979, no cases of polio caused by wild poliovirus have originated in the U.S.
- However, the wild virus has been brought into the country by travelers with polio. The last time this happened for wild poliovirus was in 1993.
It takes only one traveler with polio to bring the disease into the United States.
Recently there have been cases of polio in the state of New York. The local news agency has asked to visit with you about the situation. In preparation for the meeting your team is developing message maps on potential questions.
Use the following link with CDC to gather information for developing your message map. (https://www.cdc.gov/polio/what-is-polio/polio-us.html (Links to an external site.))
The concept of message mapping is basically an expansion of the SOCO. However, in this tool you consider all the questions that may be asked about a topic and develop a response for each question. Developing an effective message map takes a considerable amount of time. However, once developed you will have responses for multiple questions that may come up related to a public health situation or any emergency situation for that matter.
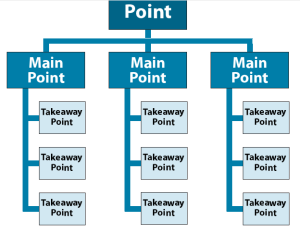
Below is the basic layout of a message map. Remember that person are best communicated to in groups of three so that is why it is built on that principal.
The following is a process used to develop the message map from ASTDR:[7]
Message Mapping Template, Worksheet, and Checklist
A message map is a useful tool for developing messages about key questions before meeting with community stakeholders. It can help you to respond to potential questions accurately and articulately.
Experts in message mapping recommend developing three main messages and three supporting messages for each of those main messages. Following the message map template are a worksheet and checklist that you can use to ensure that your messages incorporate risk communication principles and are as clear as they can be.
Message Map Template
| Communications Scenario or Issue: | ||
| Stakeholders (Interested Affected Individuals or Groups): | or | |
| Question or Concern: | ||
| Key Message 1: | ||
| Supporting Information 1: | ||
| Supporting Information 2: | ||
| Supporting Information 3: | ||
| Key Message 2: | ||
| Supporting Information 1: | ||
| Supporting Information 2: | ||
| Supporting Information 3: | ||
| Key Message 3: | ||
| Supporting Information 1: | ||
| Supporting Information 2:
Supporting Information 3: |
||
Message Review Worksheet and Checklist
When you need to develop new messages or evaluate existing ones, work through the following steps to ensure that messages are well crafted and effective.
Step 1: What is the overall topic/situation/question that you want to address (consider who, what, when, where, and how)?
Step 2: Consider the following general factors:
1. Who is the target audience(s) (e.g., general public, people living and working in the area of contamination)? What is the lowest literacy level of your target audience?
2. What is the purpose of the messages (e.g., talking points for a community meeting, a fact sheet, social media messaging, media session)?
3. What is the anticipated method of delivery (e.g., public meeting, document, one-on-one)?
Step 3: Consider what you are asking the target audience to do. Is there a specific action you are asking the target audience to perform? What is it?
Step 4: Check your messages for the following and revise them if you check “no” in any of the boxes below.
- Is the message consistent (i.e., conveys what the science tells us in the same way across messages)?
- Is the message constructed with appropriate tone and appeal (i.e., creates a sense of urgency for action, if needed; does not confuse or frighten and includes empathy, if appropriate)?
- Is the information you present understandable by your target audience (i.e., 4 years below the audience’s average grade-level education)?
- If responding to a question or comment expressing loss or stress of any kind (e.g., death, emotionally charged issue), does the response express compassion, empathy, caring, or listening first?
- Are the key messages concise (i.e., less than 27 words, 9 seconds, 3 messages)?
- Are messages free from absolutes (e.g., always, never)?
- Is the message clear (i.e., easy to understand and free from undefined jargon or acronyms)?
- Is the message focused (i.e., covers only important points and avoids extraneous information, clauses, and caveats)?
- Is the message responsive to audience concerns (i.e., information is relevant and important)?
- Are the sentences short (i.e., be no longer than 10–12 words on average)?
- Does the message map provide the most important information first and last (i.e., Primacy/Recency effects: people are more likely to accurately remember information that is presented at the beginning and end)?
- Is a negative statement or a piece of bad news balanced with at least three positive, solution-oriented, or constructive statements (1N = 3P rule: One negative equals three positives)?
Sample Message Map Worksheet
| Communications Scenario or Issue: | Is the soil in our neighborhood harmful to me and my family? |
| Stakeholders (Interested or Affected Individuals or Groups): | Public/media |
| Question or Concern: | Human health, trust in government |
| Key Message 1: | ATSDR is concerned about the soil in which you and your loved ones live, work, and play. |
| Supporting Information 1: | We are working closely with public health authorities and others to minimize any potential harm. |
| Supporting Information 2: | We are collecting samples and testing the soil from several places in the area for the presence of {insert chemical name, such as arsenic, lead, etc.} |
| Supporting Information 3: | Our scientists will determine whether touching or breathing the soil could be harmful to human health. |
| Key Message 2: | ATSDR will let you know what it finds and advise you on how you can stay safe. |
| Supporting Information 1: | People should call {insert phone number} or go to {insert Web site} for information and updates. |
| Supporting Information 2: | People should stay tuned to local television, the newspaper, or {name of social media channel}. |
| Supporting Information 3: | Until we know more, people in the impacted area {insert area} should limit their direct contact with the soil and not allow children to play in it. |
| Key Message 3: | You can limit your direct contact and exposure to the soil now through some simple behavior changes. |
| Supporting Information 1: | Wash your hands after touching soil and before preparing food, smoking, eating, or drinking. |
| Supporting Information 2: | Try to reduce soil dust in the house by leaving your shoes at the door so less soil and sediment enters your home. |
| Supporting Information 3: | Reduce outside activities that stir up dust such as digging or moving soil. |
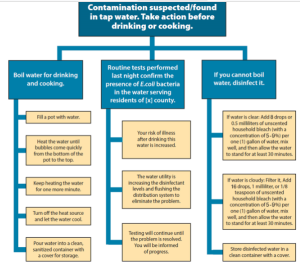
The following is an example of a message map for a drinking water problem[8]
Immediately after there Anthrax incident in the United States there was a concern that small pox could be used as a biological weapon. Small Pox was supposedly eradicated around the world certain countries kept stocks of the virus even though it was to have been destroyed. Those stocks went missing soon after the break up of the USSR. The concern was that the materials may have fallen into the hands of persons that might use Small Pox as a weapon. At the CDC they developed message maps for questions around Small Pox. Below is a partial list of the questions they developed message maps for and one map that was developed
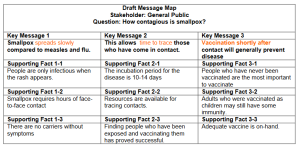
This is a partial list of the questions developed.
======================
How contagious is smallpox?
Can everyone be vaccinated?
What are the signs and symptoms of smallpox?
Who’s in charge?
Why is smallpox a good weapon?
What makes you think the strategies of the 60s and 70s will work today?
What’s being done to prepare?
What kind of medical care will be available? Is there enough?
What resources will be used to identify and respond to an outbreak?
Could terrorists make a strain that you couldn’t protect against?
Are enough resources available to care for smallpox patients?
Are laboratories able to quickly diagnose smallpox?
How do you know the new vaccine will work?
Isn’t it true that smallpox has been known to be airborne in the past?
Can I get smallpox from water, mosquitoes, pets, or farm animals?
- https://www.cdc.gov/cpr/readiness/00_docs/CDC_PreparednesResponseCapabilities_October2018_Final_508.pdf ↵
- https://www.cdc.gov/healthywater/emergency/dwa-comm-toolbox/before/tools/SOCO-Worksheet.docx ↵
- https://asprtracie.hhs.gov/technical-resources/73/social-media-in-emncy-response/77 ↵
- https://www.thewarnroom.com/ ↵
- https://www.thewarnroom.com/contents-guide ↵
- https://www.thewarnroom.com/style-guide ↵
- https://www.cdc.gov/healthywater/emergency/dwa-comm-toolbox/tools-templates-main.html ↵
- https://www.cdc.gov/healthywater/emergency/dwa-comm-toolbox/before/tools/Sample-Message-Map-508.pdf ↵