9 Infectious Disease Transmission and Outbreak Investigation
Learning Objectives
By the end of this chapter, you will be able to:
- Understand and describe infectious disease terms
- Discuss the epidemiology triangle
- Describe modes of transmission of infectious disease
Infectious Disease Terms
Infectious disease is a disease caused by an infectious agent, which includes, bacteria, viruses, fungi, parasites, and other organisms.
Contagious disease is disease that is caused by direct and indirect contact with a pathogenic or infectious agent.
Communicable disease is disease that arises from transmission of a specific infectious agent to a susceptible host.
Parasitic diseases are an infection caused by a parasite which is an animal or plant that gets nutrients by living on or in an organism of another species. A complete parasite gets its nutrients from the host organism, but a semi-parasite gets only some of its nutrients from the host (National Cancer Institute, n.d.; Centers for Disease Control and Prevention[CDC], 2012).
Infection is the entry and development of infectious agents in people, animals, or the environment.
The Epidemiologic Triangle
The epidemiologic triangle is a model used to understand health problems while understanding infectious disease and how it is spread. The three sides of the triangle include the agent, host , and the environment.
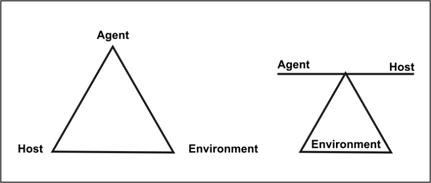
Figure 9.1: The Epidemiologic Triangle
These are two graphics that show the three sides of the epidemiologic triangle: agent, host, and environment.
The agent was originally referred to an infectious microorganism or pathogen: a virus, bacterium, parasite, or other microbe. Generally, the agent must be present for disease to occur; however, presence of that agent alone is not always sufficient to cause disease. A variety of factors influence whether exposure to an organism will result in disease, including the organism’s pathogenicity (ability to cause disease) and dose.
Over time, the concept of agent has been broadened to include chemical and physical causes of disease or injury. These include chemical contaminants (such as the L-tryptophan contaminant responsible for eosinophilia-myalgia syndrome), as well as physical forces (such as repetitive mechanical forces associated with carpal tunnel syndrome). While the epidemiologic triad serves as a useful model for many diseases, it has proven inadequate for cardiovascular disease, cancer, and other diseases that appear to have multiple contributing causes without a single necessary one.
Hosts are organisms, usually humans or animals, which are exposed to and harbor disease. A variety of factors intrinsic to the host, sometimes called risk factors, can influence an individual’s exposure, susceptibility, or response to a causative agent. Opportunities for exposure are often influenced by behaviors such as sexual practices, hygiene, and other personal choices as well as by age and sex. Susceptibility and response to an agent are influenced by factors such as genetic composition, nutritional and immunologic status, anatomic structure, presence of disease or medications, and psychological makeup.
The environment refers to extrinsic factors or favorable surroundings or conditions that affect the agent and the opportunity for exposure. Environmental factors include physical factors such as geology and climate, biologic factors such as insects that transmit the agent, and socioeconomic factors such as crowding, sanitation, and the availability of health services (CDC, 2023).
One other consideration of the epidemiologic triangle to consider is the center. The center of the triangle is time. Most infectious diseases have an incubation period known as the time between when the host is infected and when disease symptoms occur. Time can also be described as the duration of the illness or the amount of time a person can be sick before death or recovery. We can also look at time from a community public health perspective where it is described as the period from an infection to the threshold of an epidemic of a population.
The three sides of the epidemiologic triangle can also be looked at as what, who, and where or the etiology of infectious disease transmission (CDC, 2023).
The mission of epidemiologists is to break at least one side of the triangle disrupting the connection between the agent, host, and the environment.
When studying epidemiology, most infectious disease agents are microbes. Typical disease-causing microbes are bacteria, viruses, fungi, and parasites. These agents are often called microorganisms, and they live best in environments that support their growth. The environments could be water, humans, blood, and even high temperatures.
Infectious Disease Transmission
Microbes occupy all of our body surfaces, including the skin, gut, and mucous membranes. In fact, our bodies contain at least 10 times more bacterial cells than human ones, blurring the line between where microbes end and humans begin. Microbes in the human gastrointestinal tract alone comprise at least 10 trillion organisms, representing more than 1,000 species, which are thought to prevent the gut from being colonized by disease-causing organisms. Among their other beneficial roles, microbes synthesize vitamins, break down food into absorbable nutrients, and stimulate our immune systems.
The vast majority of microbes establish themselves as persistent “colonists,” thriving in complex communities within and on our bodies. In many cases, the microbes derive benefits without harming us; in other cases, both host and microbe benefit.
And though some microbes make us sick and even kill us, in the long run, they have a shared interest in our survival. For these tiny invaders, a dead host is a dead end.
The success of microorganisms is due to their remarkable adaptability. Through natural selection, organisms that are genetically better suited to their surroundings have more offspring and transmit their desirable traits to future generations. This process operates far more efficiently in the microbial world than in people. Humans produce a new generation every 20 years or so; bacteria do it every 20 to 30 minutes, and viruses even faster. Because they reproduce so quickly, microorganisms can assemble in enormous numbers with great variety in their communities. If their environment suddenly changes, the community’s genetic variations make it more likely that some will survive. This gives microbes a huge advantage over humans when it comes to adapting for survival.…
Other interventions help prevent the spread of disease by targeting the portal of entry. These strategies could include wearing personal protective equipment like disposable gloves, masks, condoms, and face shields when you are knowingly exposed to pathogens or infected individuals. Practicing proper handwashing, isolating those with infectious disease to minimize contact with others, covering coughs and sneezes, staying home when you are sick, and staying up to date on immunizations are all infection disease control efforts that allow you to take action in stopping the spread of disease (CDC, 2024).
Immunity and Immunization
Immunity to a disease is achieved through the presence of antibodies to that disease within a person’s body system. Antibodies are disease-specific, and immunity will depend on exposure.
Individuals develop immunity in one of two ways. Natural immunity is acquired from exposure to the disease organism through infection with the actual disease ( You are exposed to Varicella zoster and develop chicken pox). Or an individual gets immunized and benefits from vaccine-induced immunity (you get a varicella zoster immunization and are now protected against chicken pox exposure) which is acquired through the introduction of a killed or weakened form of the organism through immunization.
There are three types of immunity that help individuals and communities benefit from disease risks and high levels of disease. The three types of immunity are active immunity, passive immunity and herd immunity.
Active immunity occurs when exposure to a disease organism triggers the immune system to produce antibodies to that disease. Individuals’ active immunity can be acquired two ways; through natural immunity or vaccine-induced immunity. Passive immunity is provided when a person is given antibodies to a disease rather than producing them through their own immune system. Passive immunity often happens when a newborn baby acquires passive immunity from its mother’s placenta. People may also get passive immunity through immune globin antibody-containing blood products. These are often given when immediate protection from a specific disease is needed (National Centers for Immunization and Respiratory Disease, 2021).
Passive immunity is immediate whereas active immunity takes time to develop. Active immunity is much more long-lasting where passive immunity may only last a few weeks or months.
The last type of immunity is herd immunity. Herd immunity is also known as population immunity. Herd immunity is the indirect protection from an infectious disease that happens when a population is immune either through immunization or immunity developed through previous infection. According to the World Health Organization, herd immunity is best achieved through immunization. If there is herd immunity in a population, this will greatly reduce the likeliness of disease transmission from one person to another (2020).
Either way, immunity is achieved when an individual is exposed to disease in the future, their immune system will recognize it and immediately produce the antibodies needed to fight it. Active immunity is long-lasting and sometimes can last a lifetime. It is important to consider your immunity and immunization status when assessing your risk of infectious disease.
Examples of Where to find out more about Disease Outbreaks:
Take look at these links for more information on Disease Outbreaks:
- For a current list of Disease Outbreaks take a look at this link from the CDC: Current CDC Outbreaks
- Disease Outbreak News from the World Health Organization, WHO: Disease Outbreak News from the WHO
Infectious Disease Outbreak Investigation
Video Attribution: CDC NERD Academy Student Quick Learn: How is an outbreak investigated? by the Centers for Disease Control and Prevention is included in the Public Domain.
Outbreak epidemiology investigation is to study an epidemic to gain control over it and prevent the further spread of disease.
An outbreak typically is a sudden increase in the disease frequency related to place, time and population impacted. Because of thousands of outbreaks that have been reported and investigated by local health departments, public health agencies and the CDC, the spread of disease has been contained but not without impact on the observed population.
Launching an outbreak investigation requires planning and strategy. In public health epidemiologists and other public health experts use a series of steps to answer 3 key questions, “what is the problem? what is the cause? and what can we do about it?”. They use information and data to make decisions throughout an outbreak investigation. Sometimes, the data is not easy to read. So, experts use a variety of strategies and studies to try to identify the source of an outbreak and what works to control it. Because every scenario is different, it is important for them to think critically about how to interpret and use results to solve the problem (CDC, 2022; National Library of Medicine, 2010; Drexler & Institute of Medicine, 2010 ).
Epidemiologists find it useful to have a systemic approach to follow when investigating disease outbreaks. These steps can be followed when investigating disease concerns that occur locally in your community, state or multi-statewide, nationally or even across the world. These steps assure that the investigation is done quickly and proceeds without missing important steps and information.
Epidemiologic Steps of Outbreak Investigation
Outbreak investigation is an important tool used by epidemiologists to understand how often disease occurs in a population and why the disease is occurring. Through outbreak investigations, we can learn why the outbreak happened and how more cases of the disease can be controlled and prevented.
Below are the steps to an outbreak investigation along with a brief description of them from the CDC archived website:
Epidemiologic Steps of an Outbreak Investigation, found in the CDC archives at: CDC Epidemiologic Steps to Outbreak Investigation
Click on the links below and explore the information provided on the CDC webpage.
- Prepare for fieldwork
- Establish the existence of an outbreak
- Verify the diagnosis
- Construct a working case definition
- Find cases systematically and record information
- Perform descriptive epidemiology
- Develop hypotheses
- Evaluate hypotheses epidemiologically
- As necessary, reconsider, refine, and re-evaluate hypotheses
- Compare and reconcile with laboratory and/or environmental studies
- Implement control and prevention measures
- Initiate or maintain surveillance
- Communicate findings
References
Centers for Disease Control and Prevention. (2023, August 29). BAM! Body and mind. https://www.cdc.gov/healthyschools/bam/teachers.htm
Centers for Disease Control and Prevention. (2024, April 12). CDC’s core infection prevention and control practices for safe health care delivery in all settings. https://www.cdc.gov/infection-control/hcp/core-practices/index.html
Centers for Disease Control and Prevention. (2022, March 15). Investigating an outbreak. Public Health Infrastructure Center, Division of Workforce Development. https://www.cdc.gov/scienceambassador/educational/outbreak-investigation.html
National Cancer Institute. (n.d.). NCI dictionary of cancer terms. https://www.cancer.gov/publications/dictionaries/cancer-terms
National Library of Medicine (2010). How infection works. https://www.ncbi.nlm.nih.gov/books/NBK209710/
World Health Organization. (2020). Coronavirus disease (COVID-19): Herd immunity lockdowns and COVID-19. https://www.who.int/news-room/questions-and-answers/item/herd-immunity-lockdowns-and-covid-19.
Licensing and Attribution
This chapter is adapted from Chapter Two: Infectious Disease Transmission and Outbreak Investigation in Principles of Epidemiology: A Primer by Christy N. Bazan, Pedro Rodriques Curi Hallal, Rachel A. Hoopsick, Andiara Schwingel, and Rafael Miranda Tassitano and licensed CC-BY
Media Attributions
- Epidemiologic Triangle

