11 Chapter 11 – Noise and Physical Agents and The10 Essential Services of Public Health
Physical Agents
The Electromagnetic Spectrum
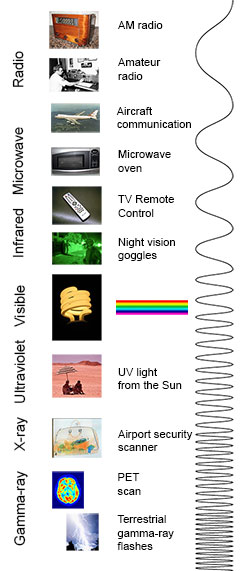
The electromagnetic (EM) spectrum is the range of all types of EM radiation. Radiation is energy that travels and spreads out as it goes – the visible light that comes from a lamp in your house and the radio waves that come from a radio station are two types of electromagnetic radiation. The other types of EM radiation that make up the electromagnetic spectrum are microwaves, infrared light, ultraviolet light, X-rays and gamma-rays.
You know more about the electromagnetic spectrum than you may think. The image below shows where you might encounter each portion of the EM spectrum in your day-to-day life.
The electromagnetic spectrum from lowest energy/longest wavelength (at the top) to highest energy/shortest wavelength (at the bottom). (Credit: NASA’s Imagine the Universe)
Radio: Your radio captures radio waves emitted by radio stations, bringing your favorite tunes. Radio waves are also emitted by stars and gases in space.
Microwave: Microwave radiation will cook your popcorn in just a few minutes, but is also used by astronomers to learn about the structure of nearby galaxies.
Infrared: Night vision goggles pick up the infrared light emitted by our skin and objects with heat. In space, infrared light helps us map the dust between stars.
Visible: Our eyes detect visible light. Fireflies, light bulbs, and stars all emit visible light.
Ultraviolet: Ultraviolet radiation is emitted by the Sun and are the reason skin tans and burns. “Hot” objects in space emit UV radiation as well.
X-ray: A dentist uses X-rays to image your teeth, and airport security uses them to see through your bag. Hot gases in the Universe also emit X-rays.
Gamma ray: Doctors use gamma-ray imaging to see inside your body. The biggest gamma-ray generator of all is the Universe.
Is a radio wave the same as a gamma ray?
Are radio waves completely different physical objects than gamma-rays? They are produced in different processes and are detected in different ways, but they are not fundamentally different. Radio waves, gamma-rays, visible light, and all the other parts of the electromagnetic spectrum are electromagnetic radiation.
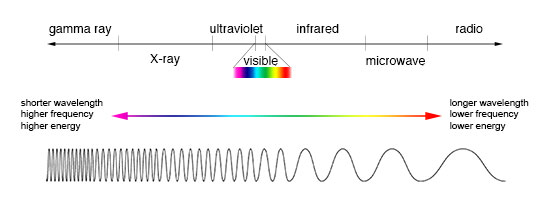
Electromagnetic radiation can be described in terms of a stream of mass-less particles, called photons, each traveling in a wave-like pattern at the speed of light. Each photon contains a certain amount of energy. The different types of radiation are defined by the the amount of energy found in the photons. Radio waves have photons with low energies, microwave photons have a little more energy than radio waves, infrared photons have still more, then visible, ultraviolet, X-rays, and, the most energetic of all, gamma-rays.
Measuring electromagnetic radiation
Electromagnetic radiation can be expressed in terms of energy, wavelength, or frequency. Frequency is measured in cycles per second, or Hertz. Wavelength is measured in meters. Energy is measured in electron volts. Each of these three quantities for describing EM radiation are related to each other in a precise mathematical way. But why have three ways of describing things, each with a different set of physical units?
The short answer is that scientists don’t like to use numbers any bigger or smaller than they have to. It is much easier to say or write “two kilometers” than “two thousand meters.” Generally, scientists use whatever units are easiest for the type of EM radiation they work with.
Astronomers who study radio waves tend to use wavelengths or frequencies. Most of the radio part of the EM spectrum falls in the range from about 1 cm to 1 km, which is 30 gigahertz (GHz) to 300 kilohertz (kHz) in frequencies. The radio is a very broad part of the EM spectrum.
Infrared and optical astronomers generally use wavelength. Infrared astronomers use microns (millionths of a meter) for wavelengths, so their part of the EM spectrum falls in the range of 1 to 100 microns. Optical astronomers use both angstroms (0.00000001 cm, or 10-8 cm) and nanometers (0.0000001 cm, or 10-7 cm). Using nanometers, violet, blue, green, yellow, orange, and red light have wavelengths between 400 and 700 nanometers. (This range is just a tiny part of the entire EM spectrum, so the light our eyes can see is just a little fraction of all the EM radiation around us.)
The wavelengths of ultraviolet, X-ray, and gamma-ray regions of the EM spectrum are very small. Instead of using wavelengths, astronomers that study these portions of the EM spectrum usually refer to these photons by their energies, measured in electron volts (eV). Ultraviolet radiation falls in the range from a few electron volts to about 100 eV. X-ray photons have energies in the range 100 eV to 100,000 eV (or 100 keV). Gamma-rays then are all the photons with energies greater than 100 keV.
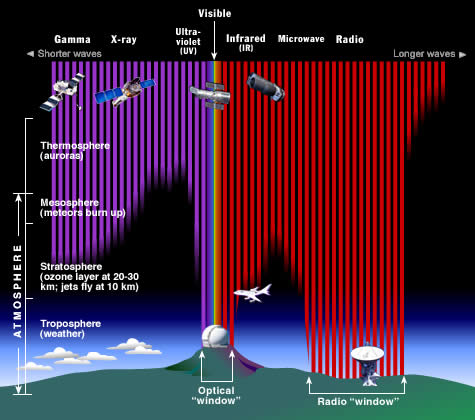
Why do we put telescopes in orbit?
The Earth’s atmosphere stops most types of electromagnetic radiation from space from reaching Earth’s surface. This illustration shows how far into the atmosphere different parts of the EM spectrum can go before being absorbed. Only portions of radio and visible light reach the surface. (Credit: STScI/JHU/NASA)
Most electromagnetic radiation from space is unable to reach the surface of the Earth. Radio frequencies, visible light and some ultraviolet light makes it to sea level. Astronomers can observe some infrared wavelengths by putting telescopes on mountain tops. Balloon experiments can reach 35 km above the surface and can operate for months. Rocket flights can take instruments all the way above the Earth’s atmosphere, but only for a few minutes before they fall back to Earth.[1]
11.02 Module 11 Discussion Concerts and Hearing Protection –Link to Blackboard Site
Pre-Discussion Work
- Health Family Team. (2018, January 2). Ears Ringing From a Loud Concert? Why That’s Not a Good Sign. Cleveland Clinic.
- Read this article that discusses damage to the ears from attending loud concerts.
Drafting Your Response
- Do you wear hearing protection when at loud concerts?
- What is your reason for your actions?
- Do you think this reading will change your actions in any way?
Discussing Your Work
What is noise-induced hearing loss?
Every day, we experience sound in our environment, such as the sounds from television and radio, household appliances, and traffic. Normally, these sounds are at safe levels that don’t damage our hearing. But sounds can be harmful when they are too loud, even for a brief time, or when they are both loud and long-lasting. These sounds can damage sensitive structures in the inner ear and cause noise-induced hearing loss (NIHL).
NIHL can be immediate or it can take a long time to be noticeable. It can be temporary or permanent, and it can affect one ear or both ears. Even if you can’t tell that you are damaging your hearing, you could have trouble hearing in the future, such as not being able to understand other people when they talk, especially on the phone or in a noisy room. Regardless of how it might affect you, one thing is certain: noise-induced hearing loss is something you can prevent.
Who is affected by NIHL?
Exposure to harmful noise can happen at any age. People of all ages, including children, teens, young adults, and older people, can develop NIHL. Based on a 2011-2012 CDC study involving hearing tests and interviews with participants, at least 10 million adults (6 percent) in the U.S. under age 70—and perhaps as many as 40 million adults (24 percent)—have features of their hearing test that suggest hearing loss in one or both ears from exposure to loud noise. Researchers have also estimated that as many as 17 percent of teens (ages 12 to 19) have features of their hearing test suggestive of NIHL in one or both ears (Pediatrics 2011
), based on data from 2005-2006.
What causes NIHL?
NIHL can be caused by a one-time exposure to an intense “impulse” sound, such as an explosion, or by continuous exposure to loud sounds over an extended period of time, such as noise generated in a woodworking shop.
Recreational activities that can put you at risk for NIHL include target shooting and hunting, snowmobile riding, listening to MP3 players at high volume through earbuds or headphones, playing in a band, and attending loud concerts. Harmful noises at home may come from sources including lawnmowers, leaf blowers, and woodworking tools.
Sound is measured in units called decibels. Sounds at or below 70 A-weighted decibels (dBA), even after long exposure, are unlikely to cause hearing loss. However, long or repeated exposure to sounds at or above 85 dBA can cause hearing loss. The louder the sound, the shorter the amount of time it takes for NIHL to happen.
Here are the average decibel ratings of some familiar sounds:
- Normal conversation
60-70 dBA - Movie theater
74-104 dBA - Motorcyles and dirt bikes
80-110 dBA - Music through headphones at maximum volume, sporting events, and concerts
94-110 dBA - Sirens
110-129 dBA - Fireworks show
140-160 dBA
Your distance from the source of the sound and the length of time you are exposed to the sound are also important factors in protecting your hearing. A good rule of thumb is to avoid noises that are too loud, too close, or last too long.

How can noise damage our hearing? (Graphic [2]
To understand how loud noises can damage our hearing, we have to understand how we hear. Hearing depends on a series of events that change sound waves in the air into electrical signals. Our auditory nerve then carries these signals to the brain through a complex series of steps.
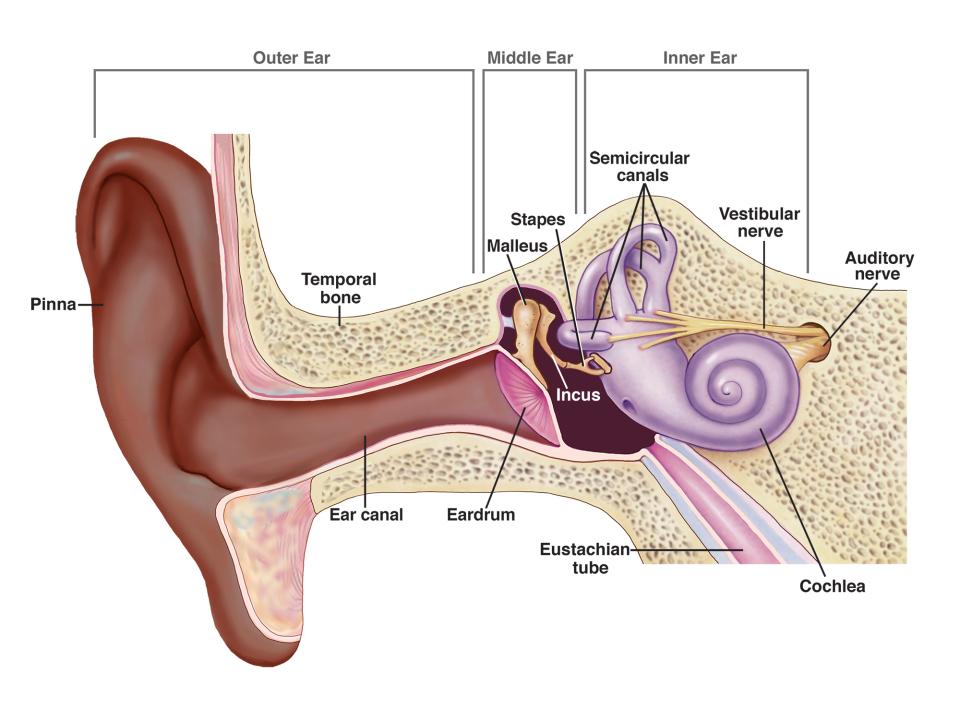
- Sound waves enter the outer ear and travel through a narrow passageway called the ear canal, which leads to the eardrum.
- The eardrum vibrates from the incoming sound waves and sends these vibrations to three tiny bones in the middle ear. These bones are called the malleus, incus, and stapes.
- The bones in the middle ear couple the sound vibrations from the air to fluid vibrations in the cochlea of the inner ear, which is shaped like a snail and filled with fluid. An elastic partition runs from the beginning to the end of the cochlea, splitting it into an upper and lower part. This partition is called the basilar membrane because it serves as the base, or ground floor, on which key hearing structures sit.
- Once the vibrations cause the fluid inside the cochlea to ripple, a traveling wave forms along the basilar membrane. Hair cells—sensory cells sitting on top of the basilar membrane—ride the wave.
- As the hair cells move up and down, microscopic hair-like projections (known as stereocilia) that perch on top of the hair cells bump against an overlying structure and bend. Bending causes pore-like channels, which are at the tips of the stereocilia, to open up. When that happens, chemicals rush into the cell, creating an electrical signal.
- The auditory nerve carries this electrical signal to the brain, which translates it into a sound that we recognize and understand.
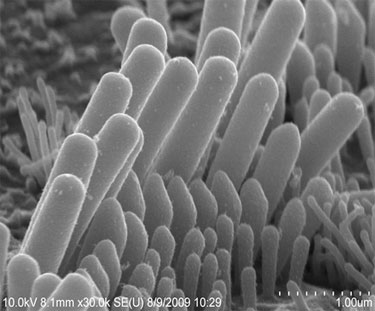
Stereocilia perch atop sensory hair cells in the inner ear.
Source: Yoshiyuki Kawashima
Most NIHL is caused by the damage and eventual death of these hair cells. Unlike bird and amphibian hair cells, human hair cells don’t grow back. They are gone for good.
What are the effects and signs of NIHL?
When you are exposed to loud noise over a long period of time, you may slowly start to lose your hearing. Because the damage from noise exposure is usually gradual, you might not notice it, or you might ignore the signs of hearing loss until they become more pronounced. Over time, sounds may become distorted or muffled, and you might find it difficult to understand other people when they talk or have to turn up the volume on the television. The damage from NIHL, combined with aging, can lead to hearing loss severe enough that you need hearing aids to magnify the sounds around you to help you hear, communicate, and participate more fully in daily activities.
NIHL can also be caused by extremely loud bursts of sound, such as gunshots or explosions, which can rupture the eardrum or damage the bones in the middle ear. This kind of NIHL can be immediate and permanent.
Loud noise exposure can also cause tinnitus—a ringing, buzzing, or roaring in the ears or head. Tinnitus may subside over time, but can sometimes continue constantly or occasionally throughout a person’s life. Hearing loss and tinnitus can occur in one or both ears.
Sometimes exposure to impulse or continuous loud noise causes a temporary hearing loss that disappears 16 to 48 hours later. Recent research suggests, however, that although the loss of hearing seems to disappear, there may be residual long-term damage to your hearing.
Can NIHL be prevented?
NIHL is the only type of hearing loss that is completely preventable. If you understand the hazards of noise and how to practice good hearing health, you can protect your hearing for life. Here’s how:
- Know which noises can cause damage.
- Wear earplugs or other protective devices when involved in a loud activity (activity-specific earplugs and earmuffs are available at hardware and sporting goods stores).
- If you can’t reduce the noise or protect yourself from it, move away from it.
- Be alert to hazardous noises in the environment.
- Protect the ears of children who are too young to protect their own.
- Make family, friends, and colleagues aware of the hazards of noise.
- Have your hearing tested if you think you might have hearing loss.
What research is being done on NIHL?
The National Institute on Deafness and Other Communication Disorders (NIDCD) supports research on the causes, diagnosis, treatment, and prevention of hearing loss. NIDCD- supported researchers have helped to identify some of the many genes important for hair-cell development and function and are using this knowledge to explore new treatments for hearing loss.
Researchers are also looking at the protective properties of supporting cells in the inner ear, which appear to be capable of lessening the damage to sensory hair cells upon exposure to noise.
The NIDCD sponsors It’s a Noisy Planet. Protect Their Hearing®, a national public education campaign to increase awareness among parents of preteens about the causes and prevention of NIHL. Armed with this information, parents, teachers, school nurses, and other adults can encourage children to adopt healthy hearing habits.[3]
Cold Stress Guide
The Occupational Safety and Health Act (OSH Act) requires employers to comply with hazard-specific safety and health standards. In addition, pursuant to Section 5(a)(1) of the OSH Act, employers must provide their employees with a workplace free from recognized hazards likely to cause death or serious physical harm. Emergency Preparedness Guides do not and cannot enlarge or diminish an employer’s obligations under the OSH Act.
Emergency Preparedness Guides are based on presently available information, as well as current occupational safety and health provisions and standards. The procedures and practices discussed in Emergency Preparedness Guides may need to be modified when additional, relevant information becomes available or when OSH Act standards are promulgated or modified.
Anyone working in a cold environment may be at risk of cold stress. Some workers may be required to work outdoors in cold environments and for extended periods, for example, snow cleanup crews, sanitation workers, police officers and emergency response and recovery personnel, like firefighters, and emergency medical technicians. Cold stress can be encountered in these types of work environment. The following frequently asked questions will help workers understand what cold stress is, how it may affect their health and safety, and how it can be prevented.
How cold is too cold?
What constitutes extreme cold and its effects can vary across different areas of the country. In regions that are not used to winter weather, near freezing temperatures are considered “extreme cold.” A cold environment forces the body to work harder to maintain its temperature. Whenever temperatures drop below normal and wind speed increases, heat can leave your body more rapidly. Cold stress is a factor of low temperature plus the wind speed plus the wetness of the individual.
Wind chill is the temperature your body feels when air temperature and wind speed are combined. For example, when the air temperature is 40°F, and the wind speed is 35 mph, the effect on the exposed skin is as if the air temperature was 28°F.
Cold stress occurs by driving down the skin temperature and eventually the internal body temperature (core temperature). This may lead to serious health problems, and may cause tissue damage, and possibly death.
What are the risk factors that contribute to cold stress?
Some of the risk factors that contribute to cold stress are:
- Wetness/dampness, dressing improperly, and exhaustion
- Predisposing health conditions such as hypertension, hypothyroidism, and diabetes
- Poor physical conditioning
How does the body react to cold conditions?
In a cold environment, most of the body’s energy is used to keep the internal core temperature warm. Over time, the body will begin to shift blood flow from the extremities (hands, feet, arms, and legs) and outer skin to the core (chest and abdomen). This shift allows the exposed skin and the extremities to cool rapidly and increases the risk of frostbite and hypothermia. Combine this scenario with exposure to a wet environment, and trench foot may also be a problem.
What are the most common cold induced illnesses/injuries?
- Hypothermia
- Frostbite
- Trench Foot
What is hypothermia?
Hypothermia occurs when body heat is lost faster than it can be replaced and the normal body temperature (98.6°F) drops to less than 95°F. Hypothermia is most likely at very cold temperatures, but it can occur even at cool temperatures (above 40°F), if a person becomes chilled from rain, sweat, or submersion in cold water.
What are the symptoms of hypothermia?
- Mild symptoms:
- An exposed worker is alert.
- He or she may begin to shiver and stomp the feet in order to generate heat.
- Moderate to Severe symptoms:
- As the body temperature continues to fall, symptoms will worsen and shivering will stop.
- The worker may lose coordination and fumble with items in the hand, become confused and disoriented
- He or she may be unable to walk or stand, pupils become dilated, pulse and breathing become slowed, and loss of consciousness can occur. A person could die if help is not received immediately.
What can be done for a person suffering from hypothermia?
- Call 911 immediately in an emergency; otherwise seek medical assistance as soon as possible.
- Move the person to a warm, dry area.
- Remove wet clothes and replace with dry clothes, cover the body (including the head and neck) with layers of blankets; and with a vapor barrier (e.g. tarp, garbage bag). Do not cover the face.
- If medical help is more than 30 minutes away:
- Give warm sweetened drinks if alert (no alcohol), to help increase the body temperature. Never try to give a drink to an unconscious person.
- Place warm bottles or hot packs in armpits, sides of chest, and groin. Call 911 for additional rewarming instructions.
- If a person is not breathing or has no pulse:
- Call 911 for emergency medical assistance immediately.
- Treat the worker as per instructions for hypothermia, but be very careful and do not try to give an unconscious person fluids.
- Check him/her for signs of breathing and for a pulse. Check for 60 seconds.
- If after 60 seconds the affected worker is not breathing and does not have a pulse, trained workers may start rescue breaths for 3 minutes.
- Recheck for breathing and pulse, check for 60 seconds.
- If the worker is still not breathing and has no pulse, continue rescue breathing.
- Only start chest compressions per the direction of the 911 operator or emergency medical services*
- Reassess patient’s physical status periodically.
*Chest compression are recommended only if the patient will not receive medical care within 3 hours.
What is frostbite?
Frostbite is an injury to the body that is caused by freezing of the skin and underlying tissues. The lower the temperature, the more quickly frostbite will occur. Frostbite typically affects the extremities, particularly the feet and hands. Amputation may be required in severe cases.
What are the symptoms of frostbite?
- Reddened skin develops gray/white patches.
- Numbness in the affected part.
- Feels firm or hard.
- Blisters may occur in the affected part, in severe cases.
What can be done for a person suffering from frostbite?
- Follow the recommendations described above for hypothermia.
- Do not rub the affected area to warm it because this action can cause more damage.
- Do not apply snow/water. Do not break blisters.
- Loosely cover and protect the area from contact.
- Do not try to rewarm the frostbitten area before getting medical help; for example, do not place in warm water. If a frostbitten area is rewarmed and gets frozen again, more tissue damage will occur. It is safer for the frostbitten area to be rewarmed by medical professionals.
- Give warm sweetened drinks, if the person is alert. Avoid drinks with alcohol.
What is immersion/trench foot?
Trench Foot or immersion foot is caused by prolonged exposure to wet and cold temperatures. It can occur at temperatures as high as 60°F if the feet are constantly wet. Non-freezing injury occurs because wet feet lose heat 25-times faster than dry feet. To prevent heat loss, the body constricts the blood vessels to shut down circulation in the feet. The skin tissue begins to die because of a lack of oxygen and nutrients and due to the buildup of toxic products.
What are the symptoms of trench foot?
- Redness of the skin, swelling, numbness, blisters
What can be done for a person suffering from immersion foot?
- Call 911 immediately in an emergency; otherwise seek medical assistance as soon as possible.
- Remove the shoes, or boots, and wet socks.
- Dry the feet.
How can cold stress be prevented?
Although OSHA does not have a specific standard that covers working in cold environments, employers have a responsibility to provide workers with employment and a place of employment which are free from recognized hazards, including cold stress, which are causing or are likely to cause death or serious physical harm to them (Section 5(a)(1) of the Occupational Safety and Health Act of 1970). Employers should, therefore, train workers on the hazards of the job and safety measures to use, such as engineering controls and safe work practices, that will protect workers’ safety and health.
Employers should train workers on how to prevent and recognize cold stress illnesses and injuries and how to apply first aid treatment. Workers should be trained on the appropriate engineering controls, personal protective equipment and work practices to reduce the risk of cold stress.
Employers should provide engineering controls. For example, radiant heaters may be used to warm workers in outdoor security stations. If possible, shield work areas from drafts or wind to reduce wind chill.
Employers should use safe work practices. For example, it is easy to become dehydrated in cold weather. Employers therefore, can provide plenty of warm sweetened liquids to workers. Avoid alcoholic drinks. If possible, employers can schedule heavy work during the warmer part of the day. Employers can assign workers to tasks in pairs (buddy system), so that they can monitor each other for signs of cold stress. Workers can be allowed to interrupt their work, if they are extremely uncomfortable. Employers should give workers frequent breaks in warm areas. Acclimatize new workers and those returning after time away from work, by gradually increasing their workload, and allowing more frequent breaks in warm areas, as they build up a tolerance for working in the cold environment. Safety measures, such as these, should be incorporated into the relevant health and safety plan for the workplace.
Dressing properly is extremely important to preventing cold stress. The type of fabric worn also makes a difference. Cotton loses its insulation value when it becomes wet. Wool, silk and most synthetics, on the other hand, retain their insulation even when wet. The following are recommendations for working in cold environments:
- Wear at least three layers of loose fitting clothing. Layering provides better insulation. Do not wear tight fitting clothing.
- An inner layer of wool, silk or synthetic to keep moisture away from the body.
- A middle layer of wool or synthetic to provide insulation even when wet.
- An outer wind and rain protection layer that allows some ventilation to prevent overheating.
- Wear a hat or hood to help keep your whole body warmer. Hats reduce the amount of body heat that escapes from your head.
- Use a knit mask to cover the face and mouth (if needed).
- Use insulated gloves to protect the hands (water resistant if necessary).
- Wear insulated and waterproof boots (or other footwear).
Safety Tips for Workers
- Your employer should ensure that you know the symptoms of cold stress.
- Monitor your physical condition and that of your coworkers.
- Dress properly for the cold.
- Stay dry in the cold because moisture or dampness, e.g. from sweating, can increase the rate of heat loss from the body.
- Keep extra clothing (including underwear) handy in case you get wet and need to change.
- Drink warm sweetened fluids (no alcohol).
- Use proper engineering controls, safe work practices, and personal protective equipment (PPE) provided by your employer.[4]
Working in Outdoor and Indoor Heat Environments
Occupational risk factors for heat illness include heavy physical activity, warm or hot environmental conditions, lack of acclimatization, and wearing clothing that holds in body heat. (See also, personal risk factors, below.)
Hazardous heat exposure can occur indoors or outdoors, and can occur during any season if the conditions are right, not only during heat waves. The following is a list of some industries where workers have suffered heat-related illnesses.
Heat-Related Illnesses and First Aid

Several heat-related illnesses can affect workers. Some of the symptoms are non-specific. This means that when a worker is performing physical labor in a warm environment, any unusual symptom can be a sign of overheating.
| Heat-Related Illness | Symptoms and Signs |
|---|---|
| Heat stroke |
|
| Heat exhaustion |
|
| Heat cramps |
|
| Heat syncope |
|
| Heat rash |
|
| Rhabdomyolysis (muscle breakdown) |
|
Employers and workers should become familiar with the heat symptoms. When any of these symptoms is present, promptly provide first aid. Do not try to diagnose which illness is occurring. Diagnosis is often difficult because symptoms of multiple heat-related illnesses can occur together. Time is of the essence. These conditions can worsen quickly and result in fatalities.
When in doubt, cool the worker and call 911.
See below for further first aid recommendations.
First Aid
OSHA’s Medical Services and First Aid standard and the Medical Service and First Aid in Construction require the ready availability of first aid personnel and equipment. First aid for heat-related illness involves the following principles:
- Take the affected worker to a cooler area (e.g., shade or air conditioning).
- Cool the worker immediately. Use active cooling techniques such as:
- Immerse the worker in cold water or an ice bath. Create the ice bath by placing all of the available ice into a large container with water, standard practice in sports. This is the best method to cool workers rapidly in an emergency.
- Remove outer layers of clothing, especially heavy protective clothing.
- Place ice or cold wet towels on the head, neck, trunk, armpits, and groin.
- Use fans to circulate air around the worker.
- Never leave a worker with heat-related illness alone. The illness can rapidly become worse. Stay with the worker.
- When in doubt, call 911!
Confusion, slurred speech, or unconsciousness are signs of heat stroke. When these types of symptoms are present, call 911 immediately and cool the worker with ice or cold water until help arrives.
Workers who are new to working in warm environments are at increased risk of heat-related illness. See the Protecting New Workers section of this website for more details. Especially during a worker’s first few days, absolutely all symptoms should be taken seriously. Workers who develop symptoms should be allowed to stop working. They should receive evaluation for possible heat-related illness.
| Outdoors | Indoors |
|---|---|
| Agriculture | Bakeries, kitchens, and laundries (sources with indoor heat-generating appliances) |
| Construction – especially, road, roofing, and other outdoor work | Electrical utilities (particularly boiler rooms) |
| Construction – roofing work | Fire Service |
| Landscaping | Iron and steel mills and foundries |
| Mail and package delivery | Manufacturing with hot local heat sources, like furnaces (e.g., paper products or concrete) |
| Oil and gas well operations | Warehousing |
Heat-related illness is preventable, especially with management commitment to providing the most effective controls. An effective heat-related illness prevention program is incorporated in a broader safety and health program and aligns with OSHA’s Recommended Practices for Safety and Health Programs core elements.
Workers who have not spent time recently in warm or hot environments and/or being physically active will need time to build tolerance (acclimatize or, less frequently used, acclimate) to the heat. During their first few days in warm or hot environments, employers should encourage workers to:
- Consume adequate fluids (water and sport drinks)
- work shorter shifts,
- take frequent breaks, and
- quickly identify any heat illness symptoms.
Engineering controls such as air conditioning, with cooled air, and increased air flow, leading to increased evaporative cooling, can make the workplace safer. Other options for keeping body temperatures down in warm environments include making changes to workload and schedules. For example, empower supervisors and workers to slow down physical activity like reducing manual handling speeds or scheduling work for the morning or shorter shifts with frequent rest breaks in the shade or at least away from heat sources. Supervisors can encourage workers in warm environments to drink hydrating fluids. At a minimum, all supervisors and workers should receive training about heat-related symptoms and first aid.
Heat-related illnesses can have a substantial cost to workers and employers. Heat stress can cause fine motor performance (like rebar tying or keyboarding) to deteriorate even in acclimatized individuals. Heat illness can contribute to decreased performance, lost productivity due to illness and hospitalization, and possibly death. OSHA encourages water, rest, and shade as prevention as well as treatment for heat-related illness.
Occupational heat exposure is a combination of many factors. Body heat results from the equilibrium of heat gain, from internal work and outside addition, and heat loss, primarily from evaporative cooling, i.e., sweat evaporation. Contributors include:
- Physical activity
- Air temperature
- Humidity
- Sunlight
- Heat sources (e.g., ovens or furnaces, heat-absorbing roofs, and road surfaces)
- Air movement
- Clothing that hampers the body’s ability to lose excess heat, such as protective gear
- Individual/personal risk factors, (e.g., pre-existing health conditions and lifestyle)
Management should commit to considering all factors that contribute to body temperature increase when determining if a heat hazard is present in a workplace. Physical activity (workload) can be estimated using tables such as this one. Employers should also be aware of whether workers’ clothing increases risk.
In addition to a thermometer, use these resources to assess heat stress:
- Use an on-site wet bulb globe temperature (WBGT) meter – the most accurate way (Morris 2018) to measure environmental heat impact on body temperature. WBGT incorporates temperature, humidity, sunlight, and air movement into a single measurement. [5]
Ionizing radiation
Ionizing radiation is radiation with enough energy that to remove tightly bound electrons from the orbit of an atom, causing that atom to become charged or ionized.
Here we are concerned with only one type of radiation, ionizing radiation, which occurs in two forms: waves or particles.
There are several forms of electromagnetic radiation, which differ only in frequency and wavelength:
- heat waves
- radio waves
- infrared light
- visible light
- ultraviolet light
- X rays
- gamma rays.
Longer wavelength, lower frequency waves such as heat and radio have less energy than shorter wavelength, higher frequency waves like X and gamma rays. Not all electromagnetic (EM) radiation is ionizing. Only the high frequency portion of the electromagnetic spectrum, which includes X rays and gamma rays, is ionizing.
Particulate radiation is a form of ionizing radiation. This consists of atomic or subatomic particles (electrons, protons, etc.) that carry kinetic energy, or mass in motion. This comes in several forms, including alpha and beta particles.
Alpha particles and beta particles are considered directly ionizing because they carry a charge and can, therefore, interact directly with atomic electrons through coulombic forces (i.e. like charges repel each other; opposite charges attract each other).
The neutron is an indirectly ionizing particle because it does not carry an electrical charge. Ionization is caused by charged particles, which are produced during collisions with atomic nuclei.
The third type of ionizing radiation includes gamma and X rays, which are electromagnetic, indirectly ionizing radiation. These are indirectly ionizing because they are electrically neutral (as are all electromagnetic radiations) and do not interact with atomic electrons through coulombic forces.
What is a dose of radiation and how is it measured?
Only the energy from ionizing radiation that is imparted to (or absorbed by) the human body can cause harm to health. To understand its biological effects, we must know (or estimate) how much energy is deposited per unit mass of the part of our body with which the radiation is interacting.
The international (SI) unit of measure for an absorbed dose is the gray (Gy), which is defined as 1 joule of energy deposited in 1 kilogram of mass. The old unit of measure for this is the rad, which stands for radiation absorbed dose. One gray is equal to 100 rads.
The biological effect of this radiation depends not only on the amount of the absorbed dose but also on the intensity of the ionization in the living cells caused by different types of radiation. This is known as the equivalent dose. For example, neutron, proton and alpha radiation can cause 5-20 times more harm than the same amount of the absorbed dose of beta or gamma radiation.
The unit of equivalent dose is the sievert (Sv). The old unit of measure is the rem. One sievert is equal to 100 rems.
Radiation is permanently present throughout the environment – in the air, water, food, soil and in all living organisms. In fact, a large proportion of the average annual radiation dose received by people results from natural environmental sources.
Each person is exposed to an average of 2.4 mSv per year of ionizing radiation from natural sources. In some areas around the world the natural radiation dose may be 5 to 10-times higher for large number of people.
Nonionizing Radiation
We use and are exposed to nonionizing radiation sources every day. Microwave ovens use microwaves to heat food, toasters use infrared waves to heat and sometimes burn our toast, and we watch television, talk on cell phones, and listen to the radio through the use of radio waves. These are all nonionizing forms of radiation. Visible light, radar, laser light, and ultraviolet light also fall into this radiation category.
Some forms of nonionizing radiation can damage tissues if we are exposed too much. For instance, too much ultraviolet (UV) light from lying out in the sun is known to cause some skin cancers; even moderate amounts can cause skin burns.
In addition to the sun, UV waves (sometimes called UV radiation) are emitted by lights used in tanning beds, black lights, and lights used to pasteurize fruit juices. Some UV waves have an energy that is high enough to cause a structural change within atoms.
Visible light waves are also a form of nonionizing radiation, as is the light beam emitted by a laser. A laser beam can be visible, as in the case of a laser pointer, or a laser can emit an invisible beam of UV or infrared waves. With enough energy, lasers can cause biological damage, which is why they are useful in medicine to remove warts and some skin cancers and even to break up kidney stones.
As we talk about these different sources, we are moving along a continuum of energy called the electromagnetic spectrum. Ionizing radiation tops the spectrum with the highest energy, nonionizing ultraviolet waves are next. Then comes visible light waves followed by infrared waves. Infrared sources in our daily lives include toasters, toaster ovens, and heat lamps.

Now we get down to the lower energies where our favorite devices operate—in the radiofrequency (RF) wave range. From highest to lowest energy, this includes microwave ovens, global positioning systems, cell phones, television stations, FM radio, baby monitors, cordless phones, garage-door openers, CB radios, and AM radio. Radiofrequency waves can cause tissue heating at high energies and with high intensities.
The last type of nonionizing radiation we’ll simply mention is extremely low-frequency (ELF) waves that are produced by electrical power lines and wiring.[6]
10 Essential Services of Public Health Summary[7]

- Monitor Health Status to Identify and Solve Community Health Problems
 Now let’s look at each of the services in more detail. This service includes accurate diagnosis of the community’s health status; identification of threats to health and assessment of health service needs; timely collection, analysis, and publication of information on healthcare access, utilization, costs, and outcomes of personal health services; and attention to the vital statistics.
Now let’s look at each of the services in more detail. This service includes accurate diagnosis of the community’s health status; identification of threats to health and assessment of health service needs; timely collection, analysis, and publication of information on healthcare access, utilization, costs, and outcomes of personal health services; and attention to the vital statistics.
Motoring conditions that influence health are decentralized across the community. Data is maintained by police on crime, drug use, and traffic-related injuries. Fire departments collect information on smoke detectors, fire-related injuries, and location of toxic chemical in the community. Hospitals have discharge and emergency services data. Schools have attendance data, student immunizations data, and graduation rates. Many other system partners have important data as well. All of this data when brought together helps describe health in the community.
This service informs decision-makers on health matters and supports selection of effective policy, plans and interventions to improve health. Efficient and effective use of computer and communication technology is needed to assure information is timely.
The question to ask yourself about this essential service:
Understand health issues at the state and community levels (Or “what’s going on in our state/community? Do we know how healthy we are?”)
2. Diagnose and Investigate Community Health Problems and Hazards
This service includes epidemiological identification of emerging health threats; public health laboratory capability using modern technology to conduct rapid screening and high-volume testing; active infectious disease epidemiology  programs; and technical capacity for epidemiological investigation of disease outbreaks and patterns of chronic disease and injury.
programs; and technical capacity for epidemiological investigation of disease outbreaks and patterns of chronic disease and injury.
This service draws heavily on epidemiology and laboratory diagnostic services. Within this service, public health and its system partners establish protocols for contact and source tracing as well as incident specific responses to address infectious disease and toxic agents found in the community. Risk assessment and hazard analysis, offered through this service, supports regulatory compliance programs and enforcement actions.
Within these protocols are specific guidance on communicating information to appropriate system partners so they can take appropriate action on diagnosis and investigation findings. Communicating to the public is implemented through EPHS 4 – the inform and educate service but it is informed by protocol from this service.
The question to ask yourself about this essential service:
Identify and respond to health problems or threats (Or “Are we ready to respond to health problems or threats? How quickly do we find out about problems? How effective is our response?”)
3. Inform, Educate and Empower People About Health Issues
 This service involves:
This service involves:
- Making health information and educational resources accessible.
- Providing health information and education activities that shape attitudes and build knowledge necessary to reduce health risk and promote better health.
- Establishing health communication plans and activities that use media advocacy and social marketing approaches to shape attitudes and build knowledge.
- Enabling informed decision-making among individuals in making health choices and among leaders establishing health policies for the community.
- Maintaining health education and promotion program partnerships with schools, faith communities, work sites, personal care providers, and others to implement and reinforce health promotion programs that shape attitudes, knowledge, skills, and behaviors needed in a healthy community population.
These activities assist to empower people to make informed decisions regarding individual and community health matters.
The question to ask yourself about this essential service:
Keep people informed about health issues and healthy choices. (Or “How well do we keep all people and segments of our State informed about health issues?”)
4. Mobilize Communities to Identify and Solve Community Health Problems
Community health improvement is a collaborative effort requiring:
- Skilled conveners and organizers,
- Social responsiveness (above self-interest) from community members, and
- System structures that link community assets and the public’s will to act.
One person or organization can start community change, but neither can make change alone. It is critical for public health system leaders to effectively convene and organize for community actions that can improve health.
Actions within the public health system that demonstrate this service are:
- Convening and facilitating multiple community groups to undertake health improvement work. Convener should seek to include those that are not typically considered to be involved in health-related matters. Mobilized groups can undertake defined preventive, screening, and rehabilitation initiatives, or support other programs activities that influence health.
- The building of coalition is one form or system to facilitate collaboration. Other forms exist. The key however is that structures must be maintained to support the mobilization of the community in order to draw upon the full range of community assets including people, organizations, and the physical environment that can support the improvement of health.
Many broadly focused processes of community action exist across the U.S. under names like Healthy Communities, Livable Communities, and Loveable Communities. An even greater number of issue specific processes exist and are addressed under names such as Healthy Mothers and Babies, Mother’s Against Drunk Driving, and many, many other collaborative groups taking action to address environmental, economic, historical, and other efforts that can improve community health and quality of life.
The question to ask yourself about this essential service:
Engage people and organizations in health issues. (Or “How well do we really get people and organizations engaged in health issues?”)
5. Develop Policies and Plans That Support Community Health Efforts
 Policies addressing specific health-related issues are public statements establishing directions individuals, organizations, or governments follow to protect and promote health. Policies are established by organizations and governments to identify consistent behaviors that are expected. Community and organization leaders have responsibility to articulate policies built on proven scientific finding and shaped by community values. Policies having negative or positive influences on health touch every aspect of community life. Safety standards that makers of automobiles and producers of electrical materials follow demonstrate policies that protect people from injury. Food handling guidelines protect people from illness. Other policy examples designed to encourage or support healthy behaviors can be identified in zoning rules. For example, zoning that requires sidewalks in new residential developments. This type of policy has influence on health by supporting the opportunity for physical activity as well as improving pedestrian safety. In addition, organizational leaders can influence health with policies that govern use of tobacco at company facilities, the availability of health insurance for employees, or facilities and time that allow for and promote physical activity. These are all examples of health-related policies that are important for community leaders to understand and apply. How well is health-related policy used to improve health in our community?
Policies addressing specific health-related issues are public statements establishing directions individuals, organizations, or governments follow to protect and promote health. Policies are established by organizations and governments to identify consistent behaviors that are expected. Community and organization leaders have responsibility to articulate policies built on proven scientific finding and shaped by community values. Policies having negative or positive influences on health touch every aspect of community life. Safety standards that makers of automobiles and producers of electrical materials follow demonstrate policies that protect people from injury. Food handling guidelines protect people from illness. Other policy examples designed to encourage or support healthy behaviors can be identified in zoning rules. For example, zoning that requires sidewalks in new residential developments. This type of policy has influence on health by supporting the opportunity for physical activity as well as improving pedestrian safety. In addition, organizational leaders can influence health with policies that govern use of tobacco at company facilities, the availability of health insurance for employees, or facilities and time that allow for and promote physical activity. These are all examples of health-related policies that are important for community leaders to understand and apply. How well is health-related policy used to improve health in our community?
Health plans provide strategic and operational guidance on how to improve health. Plans establish a set of objectives and related actions to make measurable health improve. Community health plans are more likely to be accepted and applied if the plans are made with the active participation of those the plans affect. Establishing a community health improvement plan builds on other essential services that result in development of good community health data, use of relevant public health science in decision-making, effective community education, establishment of supportive health-related policies, and mobilization efforts necessary to bring about health improvements. Community health improvement is not limited to issues classified within traditional public health or health services categories, but may include environmental, business, economic, housing, land use, and other community issues indirectly affecting the public’s health.
This service represents decision-making and action to plan and measure general community health improvement. In addition, this essential service addresses more specific health plans like those that focus on preparation and response to disasters and all the human health and environmental implications resulting from disasters.
The question to ask yourself about this essential service:
Plan and implement sound health policies. (Or “What policies promote health in our State? How effective are we in planning and in setting health policies?”)
6. Enforce Laws, Regulations, and Rules That Protect Health and Ensure Safety
Governmental officials form public health and other regulatory officials have responsibility to assess legal authority  and effectiveness of regulations. If regulations are not based on appropriate public health science and contemporary practice standards or if there are new regulations needed to properly protect health, public health leaders should advocate for needed regulator change. The primary purpose of health-related regulation is not punishment but compliance. Public health should employ the use of education and other methods to enable individuals and organizations to comply with health and safety regulations. If there is failure to comply, it is essential that public health use its enforcement authority to protect the public.
and effectiveness of regulations. If regulations are not based on appropriate public health science and contemporary practice standards or if there are new regulations needed to properly protect health, public health leaders should advocate for needed regulator change. The primary purpose of health-related regulation is not punishment but compliance. Public health should employ the use of education and other methods to enable individuals and organizations to comply with health and safety regulations. If there is failure to comply, it is essential that public health use its enforcement authority to protect the public.
Compliance and enforcement areas for public health include sanitary codes, especially in the food industry; protection of drinking water supplies; enforcement of clean air standards; protection from toxic and physical hazards in the environment; and monitoring the quality of medical services delivered through facilities such as laboratories, nursing homes, and home healthcare agencies.
The question to ask yourself about this essential service:
Enforce public health laws and regulations. (Or “When we enforce health regulations are we up-to-date, technically competent, fair and effective?”
7. Link People to Personal Health Services
 This service (often referred to as the “outreach” or “enabling” service) includes assuring effective entry of people into a coordinated system of clinical care, especially the socially disadvantaged. This may involve identifying and addressing potential barriers related to cultural, language of materials, or staff serving special population groups. It most certainly involves providing people access and linkage to a coordinated system of personal healthcare that provides ongoing “care management,” transportation services, and targeted health information to high-risk population groups. The system should also ensure delivery of effective health promotion and disease prevention services within the community as well as provision of technical assistance to community providers who wish to improve or offer health promotion services.
This service (often referred to as the “outreach” or “enabling” service) includes assuring effective entry of people into a coordinated system of clinical care, especially the socially disadvantaged. This may involve identifying and addressing potential barriers related to cultural, language of materials, or staff serving special population groups. It most certainly involves providing people access and linkage to a coordinated system of personal healthcare that provides ongoing “care management,” transportation services, and targeted health information to high-risk population groups. The system should also ensure delivery of effective health promotion and disease prevention services within the community as well as provision of technical assistance to community providers who wish to improve or offer health promotion services.
The question to ask yourself about this essential service:
Make sure people receive the medical care they need. (Or “Are people receiving the medical care they need?”)
8. Assure a Competent Public and Personal Health Care Workforce
This service includes:
- Education and training for personnel to meet the needs for public and personal health service.

- Efficient processes for licensure of professionals and certification of facilities with regular verification and inspection follow-up.
- Adoption of continuous quality improvement and life-long learning within all licensure and certification programs.
- Active partnerships with professional training programs to assure community-relevant learning experiences for all students; and
- Continuing education in management and leadership development programs for those charged with administrative or executive roles.
Actions to achieve the intent of this service may include assessing the supply and competencies of those providing person healthcare and public health services. Assuring health workers are properly trained and recognized by licensure or other credentialing processes. Supporting access to a system for life-long learning to maintain and grow health worker competencies, including the provision of mentors who can cultivate leadership and cultural competencies within the workforce.
The question to ask yourself about this essential service:
Maintain a competent public health and medical workforce. (Or “Do we have a competent public health staff? How can we be sure that our staff stays current?”)
9. Evaluate Effectiveness, Accessibility, and Quality of Health Services
 This service calls for ongoing evaluation of health programs, based on analysis of health status and service utilization data, to assess program effectiveness and to provide information necessary for allocating resources and reshaping programs.
This service calls for ongoing evaluation of health programs, based on analysis of health status and service utilization data, to assess program effectiveness and to provide information necessary for allocating resources and reshaping programs.
Its through this service we should answer the questions
- Are we doing things, right? and
- Are we doing the right things to effectively improve health?
Evaluation must be seen as a consistent part of all public health work. Evaluation can be identified in many forms such as customer service feedback, quality improvement programs that examine the process of service delivery, or rigorous case control evaluation. All levels of evaluation are needed. Evaluation is needed for effective decision-making and resource allocation. It is through evaluation that we understand our improvements.
This service includes continuous linkage with appropriate institutions of higher learning and research and an internal capacity to mount timely epidemiological and economic analyses and conduct needed health services research.
Public health professionals have great opportunity to develop new information needed to better understand how community health can be improved. Necessity often requires innovative solutions to the health problems State and local public health professionals face. Most of our health service advances originated from the experience and insight of frontline public health workers and confirmed in collaboration study with health researchers. Public health at the State and local level must develop the capacity to participate in and guide health services research. Linkages must be established with research and academic centers in order to stimulate and capture new insights and innovations we need to public health problems. Such research must be fully participatory with those it studies and intend to affect.
The question to ask yourself about this essential service:
Evaluate and improve programs and . (Or “Are we doing any good? Are we doing things, right? Are we doing the right things?”) plus Support innovation and identify and use best practices. (Or “Are we discovering and using new ways to get the job done?”)
10. Building a strong organizational infrastructure for public health.
Developing an understanding of the broader organizational infrastructures and roles that support the entire public  health system in a jurisdiction (e.g., government agencies, elected officials, and non-governmental organizations). In this we need to ensure that appropriate needed resources are allocated equitably for the public’s health. This really speaks to developing appropriate strategic plans that are based upon the monitoring and needs assessments for a community.
health system in a jurisdiction (e.g., government agencies, elected officials, and non-governmental organizations). In this we need to ensure that appropriate needed resources are allocated equitably for the public’s health. This really speaks to developing appropriate strategic plans that are based upon the monitoring and needs assessments for a community.
Governance is crucial for implementing any plan to be effective. Policy makers need to be appropriately trained similar to training provided by the National Association of Local Boards of Health and the National Association of City and County Health Officials. Both of these organizations provide training for board members that speaks to governance and leadership in the area of public health.
Public health entities need to properly manage their financial resources and direct their efforts toward the identified health needs within a community. They also need to hire the appropriate human resources to deliver the programs.
The public health entities need to provide for their staff and the community a robust information technology that meets privacy and security standards. In this day there is an expectation of the community that social media will play an integral part of proper communication.
This service anticipates that all parties concerned will be accountable, transparent and inclusive and with the community. Nothing erodes trust within a partnership than lack of transparency.
The question to ask yourself about this essential service:
Building and maintaining a strong organizational infrastructure for Public Health ( Or. “Are we really playing well with all of our partners for the best of our community”)
- https://imagine.gsfc.nasa.gov/science/toolbox/emspectrum1.html ↵
- https://www.shponline.co.uk/wp-content/uploads/2015/10/hearing-loss-noise-levels.jpg ↵
- https://www.nidcd.nih.gov/health/noise-induced-hearing-loss ↵
- https://www.osha.gov/emergency-preparedness/guides/cold-stress ↵
- https://www.osha.gov/heat-exposure ↵
- https://www.radiationanswers.org/radiation-introduction/types-of-radiation/non-ionizing-radiation.html ↵
- https://phnci.org/uploads/resource-files/EPHS-English.pdf ↵