13 Chapter 13 – Impact of Temperature Change on Health and Clean Energy Alternatives,
Impact of Temperature Change on Health
The influence of the winter North Atlantic Oscillation index on hospital admissions through diseases of the circulatory system in Lisbon, Portugal[1]
The aim of this paper is to analyze the relationship between North Atlantic Oscillation (NAO), meteorological variables, air pollutants, and hospital admissions due to diseases of circulatory systems in Lisbon (Portugal) during winter months (2003–2012). This paper is one of the few studies analyzing the impact of NAO on health through its influence on thermal stress and air pollution and is the first to be conducted in Lisbon. This study uses meteorological data (synthetized into a thermal comfort index), air pollutant metrics, and the NAO index (all clustered in 10-day cycles to overcome daily variability of the NAO index). The relationship between morbidity, thermal comfort index, NAO index, and air pollutants was explored through several linear models adjusted to seasonality through a periodic function. The possible indirect effect between the NAO index and hospital admissions was tested, assuming that NAO (independent variable) is affecting hospital admissions (outcome variable) through thermal discomfort and/or pollution levels (tested as individual mediators). This test was conducted through causal mediation analysis and adjusted for seasonal variation. The results from this study suggest a possible indirect relationship between NAO index and hospital admissions. Although NAO is not significantly associated with hospital admissions, it is significantly associated with CO, PM2.5, NO, and SO2 levels, which in turn increase the probability of hospitalization. The discomfort index (built with temperature and relative humidity) is significantly associated with hospital admissions, but its variability is not explained by the NAO index. This study highlights the impacts of the atmospheric circulation patterns on health. Furthermore, understanding the influence of the atmospheric circulation patterns can support the improvement of the existing contingency plans.
This study assesses the influence of NAO on health in Lisbon (during the winter months from 2003 to 2012). The results from this analysis show a possible indirect relationship between NAO and hospital admissions from circulatory diseases. This relationship is established through the indirect effect of pollution: NAO is associated with CO, PM2.5, NO, and SO2 levels, which in turn increase the probability of hospitalization. Hospital morbidity significantly increases with thermal stress (the DI is significantly associated with hospital morbidity due to diseases of the circulatory system diseases), although, thermal stress is not explained by the NAO index. Previous studies conducted in Europe have shown the effects of NAO on health. Messner et al. (2003) found a consistent positive relation between increasing NAO index and an increase in acute myocardial mortality in Sweden. Hubálek (2005) analyzed the impact of NAO on the incidence of some infectious diseases in the Czech Republic and found significant correlations between them. McGregor (2005) found statistically significant inverse associations between mortality from ischemic heart disease and the climate index representing the interaction between the NAO and temperature across England. Pausata et al. (2013), assessing the particulate matter variability induced by NAO in Europe during winter and the potential impact on human health, found that positive shift in the mean winter NAO of one standard deviation would lead to about 5500 additional premature deaths in Mediterranean countries due to the increase in particulate matter concentration.
Nevertheless, as described above, we found significant positive linear associations between the NAO index and CO, PM2.5, NO, and NO2. Similar results were also mentioned by Jerez et al. (2013) and Christoudias et al. (2012) which reported lower concentration of pollutants in southern Europe during NAO negative phases. These results show the processes of transport and deposition of air pollutants through the effect of wind and precipitation.
Air pollutants are positively associated with hospital admissions (except O3 and NO2); previous studies analyzing the health impact of several air pollutants also reported important differences between them: Forastiere et al. (2005), in Rome, identified significant increases of out-of-hospital coronary deaths with CO and PM10, but not with NO2; Cendon et al. (2006) found stronger positive correlations between SO2 and daily hospitalizations for myocardial infarctions than between CO, O3, NO2, and PM10.
O3 is negatively associated with hospital admissions; however, there is no causal relationship between the decreasing levels of ozone and the hospital admission increase. This apparent protective effect results from the O3 increase on warm days, while the relation between hospital admissions and temperature is inverse (Moolgavkar et al. 1995, Ito et al. 2005, Medina-Ramón et al. 2006). Similar results were found in the previous research (Moolgavkar et al. 1995, Medina-Ramón et al. 2006).
The thermal comfort index is not significantly associated with the NAO index. Unlike the countries of Central and North Europe where a strong association is found between the NAO index and temperature (Osborn et al. 1999, Trigo et al. 2002, Hurrell et al. 2003), in Lisbon, this relationship was not recorded. The results of this study are supported by the study of Ulbrich et al. (2012), showing that the relationship between the NAO index and temperature is not linear in the Iberian Peninsula.
Summarizing, hospital morbidity is positively associated with the pollutant levels (except ozone and NO2, as reported previously) and is negatively associated with the thermal comfort index, although no significant direct association with NAO was found. A similar pattern was also found in previous studies addressing vulnerability to cold weather (Almendra et al. 2012, 2016, Vasconcelos et al. 2013) or exposure to high levels of air pollution (Borrego et al. 2009, Slezakova et al. 2011) in Portugal.
Strengths and limitations
This study is one of the few analyzing the impact of NAO on health and is the first to be conducted in Lisbon. Considering the geographical and socioeconomic context of Portugal and the high vulnerability to harmful environmental conditions is fundamental to have a better understanding of the relationship between atmospheric conditions and health to effectively assess environmental risks. Thus, this study represents an important contribution to the current body of literature.
However, the results of this study must be interpreted with caution. Time series analyses were carried out for one location as such; the results should not be derived to other regions with different geographic and socioeconomic frameworks.
The methods applied in this study tested for direct and indirect linear associations; however, the relationship between environmental conditions and health is often studied by nonlinear modeling providing better fitting models. Therefore, the linear mediation model is an alternative to (direct) nonlinear models and can also be employed as an exploratory and complementary tool to those models.
Conclusions
This study investigated the effects of NAO on emergency hospital admissions from diseases of the circulatory system during the winter months in Lisbon. It was found that the NAO influences human health through its impacts on atmospheric pollutants. Positive NAO phases are associated with higher levels of air pollutants. No significant association was found between NAO and the discomfort index (built with temperature and relative humidity).
Although it is not possible to extrapolate from this to other countries or other areas of Portugal, this study draws attention to the impacts of the patterns of atmospheric circulation in the North Atlantic on human health and to the vulnerability to environmental factors.
This article can provide insights to improve public health policies and alert systems. A better understanding of the relationship between the NAO and health can help improve existing contingency plans, develop more effective adaptation strategies, and ensure they are put into action in a timely manner, thereby helping to decrease the health impacts of harmful environmental conditions.
Temperature effects on health – current findings and future implications[2]
Heat waves and cold spells have both shown adverse effects on mortality. Moreover, a recent study by Gasparrini and colleagues estimated that 7.7% of the mortality was attributable to non-optimum temperature using data from 384 locations (Gasparrini et al. 2015). Cold was responsible for a higher proportion of deaths than was heat, while moderate high and low temperatures represented most of the total health burden. Although forecasting studies suggest the passage of (summertime) cold fronts will diminish in frequency in a warmer climate, this will not per se mean that cold effects will only have a very small effect on population health. Studies have already shown that health effects associated with temperature decreases in winter and summer can be similar in magnitude but are more pronounced in years with higher average temperatures. Therefore, the influence of unexpected temperature changes may be more relevant than the absolute temperature level itself (Shi et al., 2015, Wolf et al., 2009).
Populations worldwide are rapidly ageing. The age group 60 years and older is expected to comprise 21.1% of the population by 2050 (http://www.un.org/en/development/desa/population/publications/ageing/WorldPopulationAgeingReport2013.shtml). This increase in the elderly is expected to increase future temperature-related mortality and morbidity.
Recent reviews have contributed to the evidence on the association between air temperature and mortality and morbidity (Aström et al., 2011, Franchini and Mannucci, 2015, Phung et al., 2016, Ryti et al., 2016, Turner et al., 2012, Yu et al., 2012). However, these reviews were limited by either a focus on only heat or cold, a specific outcome, or did not include a meta-analysis. Only two of them presented age-specific results.
The purpose of the systematic review and meta-analyses by Bunker et al. was to present quantitative evidence on the effects of non-optimum high and low ambient temperatures on a range of cause-specific mortality and morbidity outcomes in the elderly (Bunker et al. 2016). Heat waves and cold spells were excluded because they are unique events with differing characteristics. Epidemiological time-series and case-crossover studies reporting quantitative associations between temperature and cause-specific, elderly mortality or morbidity (i.e. hospitalization, emergency room admissions, general practice visits, home visits) were considered.
The authors identified substantially elevated risks in the elderly for temperature-induced cerebrovascular, cardiovascular, and respiratory outcomes in particular. In their meta-analysis for morbidity, the authors showed that the effect estimates for respiratory causes were much larger than for cardiovascular causes with both, high and low temperatures – although for mortality, the effect estimates for cardiovascular causes were similar or slightly larger than for respiratory causes in case of high temperatures. This phenomenon has been already shown in previous studies (e.g. Michelozzi et al. 2009). However, the underlying mechanisms through which high temperatures may increase the risk of morbidity from respiratory causes are yet unclear. In addition, Bunker et al. found an increased risk for heat-induced diabetes, renal, and infectious disease morbidity all of which are likely to increase further with climate change and global aging.
The authors had to pool across different lags and threshold temperatures of the various studies. Therefore, the important fact that the effects of heat are most often immediate while the ones of cold become predominant with longer time lags is not obvious in their pooled effects tables. This limitation was overcome by sensitivity analyses (e.g. for certain lags) where possible.
The systematic review and meta-analysis by Bunker et al. is timely and helpful for pointing out further research needs and possible public health interventions especially for the elderly.
Climate change does not just affect air temperatures, but also a lot of other meteorological variables which might be as important to human health as temperature changes, such as humidity, barometric pressure and precipitation as well as UV-radiation. In addition, it is still unclear why outdoor temperature changes show consistent health effects across all geographical regions despite the fact that especially the elderly spend most of their time indoors. Moreover, the interplay with air pollution is quite complex and new multicenter studies as well as statistical approaches are needed. With an aging population, mental health and cognitive function in particular is an emerging field of concern (Lacruz et al. 2010) in which environmental stressors certainly play a role.
According to the European Environment Agency (http://www.eea.europa.eu/soer/synthesis/synthesis), about 75% of the European population lives in urban areas and is projected to increase to 80% by 2020. Urbanization has resulted in improved access to education, employment and health care. However, it also changed living conditions and influences lifestyles, behaviors and environmental conditions. Urban heat islands were identified as contributing significantly to the health impact of the 2003 heat wave in Paris (Laaidi et al. 2012). Further, it has been projected that a reduction of the green cover by 10% would increase urban temperatures by 8.2°C over the next 70 years (Gill et al. 2007) – highlighting the potential for improving health and well-being by measures improving the built environment.
What was the impact of the Dust Bowl?
During the 1930s, the Midwest experienced so much blowing dust in the air that the region became known as the Dust Bowl. The term also refers to the event itself, usually dated from 1934 through 1940. The heart of the Dust Bowl was the Texas panhandle and western Oklahoma, but atmospheric winds carried the dust so far that East Coast cities sometimes found a powdery layer of dirt on windows, streets, sidewalks and automobiles. On the Great Plains, however, dust storms were so severe that crops failed to grow, livestock died of starvation and thirst and thousands of farm families lost their farms and faced severe poverty.
Factors of the Dust Bowl
Most authorities cite two factors as the cause of the Dust Bowl. In the 1920s, with the coming of tractors and mechanical farm implements, farmers on the Great Plains plowed up huge tracts of land once covered with grasses that held the soil in place and helped to keep in moisture in the topsoil. Without the grass cover, the wind could lift dirt particles into the atmosphere where they were carried east by the prevailing winds. During the summers of 1934, 1936 and 1939-40, little rain fell, creating drought conditions in Iowa and across the Midwest. Extreme high temperatures topped 100 degrees sometimes for weeks at a time. Crops withered in the field and again, the soil was left with no cover to prevent the topsoil from blowing into the air.
The result was that the huge clouds of dust formed, often so strong that they blocked the sun creating darkness and limited visibility even during the day. Even when families stuffed rags under the doors and around the windows, dust filtered into homes covering everything. One woman recalled that when she sat up in the morning, she could see the silhouette of her head outlined in dust on her pillow.
The Dust Bowl and The Great Depression
The extreme weather came on top of farmers struggling to survive during the Great Depression. Guaranteed high prices during WWI and government appeals to farmers’ patriotism encouraged many to expand their herds and their cropland. When the war ended and demand for extra production fell, farmers continued to produce at record levels. Surpluses developed, and farm prices fell sharply making many farmers unable to pay their mortgages. Farm foreclosures across the Midwest skyrocketed and the situation looked desperate. Franklin Roosevelt’s New Deal boosted farm prices by paying farmers to limit production. While those programs were just beginning, however, the drought years of 1934 and 1936 made life even more difficult for farm families and the small towns that depended upon them. In Oklahoma and nearby regions, many families joined a mass migration to California, piling up whatever they could onto their automobiles. They became known as the “Okies.”
Conservation Efforts
The Dust Bowl taught the United States to explore better approaches to land management. Western lands with too little rainfall to support grain crops like corn or wheat should be left as pasture to maintain a grass cover that can retain moisture and keep topsoil in place. The federal government began support for programs to plant trees as windbreaks, to terrace hillsides, and to implement other land management programs. It also produced a famous film, “The Plow That Broke the Plains,” that dramatically illustrated the relationship between farming practices and the Dust Bowl.
Both weather and human efforts contributed to the Dust Bowl. Iowans who lived it remember the frightening appearance of dark clouds of descending dirt. They suffered through it but also learned some valuable lessons about the need to respect the natural environment.[3]
The homeowner’s severe cold weather survival guide
Much of North America experiences periods of severely cold weather and is susceptible to snow and ice storms—extreme conditions that can inflict considerable damage on homes and create liability risks. Standard homeowners policies will cover most disasters that result from a freeze—but when the weather outside is frightful, it’s better to minimize the potential risks. Here’s how.
Inside the house
If you’ve prepped your house for the winter weather, you’re ahead of the game. When the temperature actually drops, here are a few more steps to take.
- Keep your house heated to a minimum of 65 degrees. The temperature inside the walls where the pipes are located is substantially colder than the walls themselves. A temperature lower than 65 degrees might not keep the inside walls from freezing.
- Check the location for the main water shutoff in your home. And refresh your memory on—or learn—how it works, in case you have to use it.
- Open hot and cold faucets enough to let them drip slowly. In severely frigid temperatures, keeping water moving within the pipes will help prevent freezing.
- Check that fireplaces, wood stoves and electric heaters are working properly. Make sure there are no combustible items near the heat sources and watch them closely, especially the first time in the season you use them.
- Keep your fireplace flue closed when you’re not using it.
- Ask a neighbor to check the house regularly any time you’re away. If pipes freeze or if there’s a water leak, quick action could mean far less damage. If you plan to be away for an extended period of time, have the water system—including swimming pool plumbing, if applicable—drained by a professional to keep pipes from freezing or bursting.
Outside the houseThe weight of snow could damage your roof. Backed-up gutters might allow water to seep into your house. Vigilance is key during severe weather—stay ahead of the potential hazards outside your home.
- Keep sidewalks and entrances to your home free from snow and ice. You don’t want anyone to slip and fall.
- Watch for ice dams near gutter downspouts. Ice dams can cause water to build up and seep into your house. Clear gutters of leaves and debris to allow runoff from melting snow and ice to flow freely.
- Run your swimming pool pump at night when the temperatures are expected to go below freezing. This will keep the water flowing through the pipes.
- Keep your garage doors closed. This will prevent weather damage to whatever’s stored in there. Plus, if your garage is attached to your house, the home entrance door from the garage is probably not as well insulated as an exterior door so this will keep more heat in.
- Double check for dead, damaged or dangerous tree branches and have them removed. Even if they looked sound earlier in the year, trees can be affected by ice, snow or wind. When stressed, branches can fall and damage your house or car, or injure someone on or near your property.
In the event of a problemSometimes the unfortunate happens—but quick action can minimize the damage. And if you have a standard homeowners insurance policy, it’s likely you’re covered for most deep freeze disasters.
- Don’t wait for frozen pipes to burst. If your pipes are frozen, take measures to thaw them immediately, or call a plumber for assistance.
- If your pipes burst, first turn off the water. You know now where the main water shut off is, right? Cut off the flow, then attend to the mess and …
- Properly dry and repair any water damage. This will help prevent any potential problems with mold.
- Call your insurance professional as soon as possible. He or she will help you understand what’s covered by your policy. And familiarize yourself with the claims filing process.
Clean Energy Alternatives
What is LEED?
LEED system goals
LEED is a holistic system that doesn’t simply focus on one element of a building such as energy, water or health, rather it looks at the big picture factoring in all of the critical elements that work together to create the best building possible. The goal of LEED is to create better buildings that:
Reduce contribution to
global climate change
Enhance individual human health
Protect and restore water resources
Protect and enhance biodiversity
and ecosystem services
Promote sustainable and
regenerative material cycles
Enhance community quality of life[4]
Of all LEED credits, 35% of the credits in LEED are related to climate change, 20% of the credits directly impact human health, 15% of the credits impact water resources, 10% of the credits affect biodiversity, 10% of the credits relate to the green economy, 5% of the credits impact community and 5% of the credits impact natural resources. In LEED v4.1, a majority of the LEED credits are related to operational and embodied carbon.
LEED is a third-party green building certification program and the globally recognized standard for the design, construction and operation of high-performance green buildings and neighborhoods. The rating system approach focuses on efficiency and leadership to deliver the triple bottom line returns of “people, planet and profit.”
Appropriate for all building types and phases, including new construction, interior fit-outs, operations and maintenance, and core and shell, LEED gives building owners and operators the tools they need to have an immediate and measurable effect on the performance of their spaces.
By promoting a whole-building approach to sustainability, LEED recognizes achievements in location and planning, sustainable site development, water savings, energy efficiency, materials selection, waste reduction, indoor environmental quality, innovative strategies and attention to priority regional issues.
How are the rating systems structured?
The LEED rating systems are made up of prerequisites and credits. Prerequisites are required elements or green building strategies that must be included in any LEED-certified project. Credits are optional elements that projects can pursue to gain points toward LEED certification.
Although the organization of prerequisites and credits varies slightly depending on the building type and associated rating system, LEED is generally organized by the following broad concepts:
- Integrative process
- Location and transportation
- Sustainable sites
- Water
- Energy
- Materials and resources
- Indoor environmental quality
How does a project achieve certification?
Achieving LEED certification requires satisfying all prerequisites and earning a minimum number of credits. Reference guides, designed to help project teams, explain credit criteria, describe the benefits of complying with the credit and suggest approaches to achieving credit compliance. The levels of certification generally follow these thresholds:
- Certified: 40–49 points
- Silver: 50–59 points
- Gold: 60–79 points
- Platinum: 80+ points
Going above and beyond
In a world facing unprecedented challenges in terms of health, water scarcity, air quality, resilience and climate change, LEED Positive is USGBC’s long-term regenerative design vision for green building. This vision that will help us push the market beyond lessening the negative impact of buildings to reaching a future that allows buildings, cities and communities to become vehicles of restoration and repair.[5]
Energy Efficient Alternative to heating and Cooling
Heat pumps offer an energy-efficient alternative to furnaces and air conditioners for all climates. Like your refrigerator, heat pumps use electricity to transfer heat from a cool space to a warm space, making the cool space cooler and the warm space warmer. During the heating season, heat pumps move heat from the cool outdoors into your warm house. During the cooling season, heat pumps move heat from your house into the outdoors. Because they transfer heat rather than generate heat, heat pumps can efficiently provide comfortable temperatures for your home.
Ducted Air-Source Heat Pumps
There are three main types of heat pumps connected by ducts: air-to-air, water source, and geothermal. They collect heat from the air, water, or ground outside your home and concentrate it for use inside.
The most common type of heat pump is the air-source heat pump, which transfers heat between your house and the outside air. Today’s heat pump can reduce your electricity use for heating by approximately 50% compared to electric resistance heating such as furnaces and baseboard heaters. High-efficiency heat pumps also dehumidify better than standard central air conditioners, resulting in less energy usage and more cooling comfort in summer months. Air-source heat pumps have been used for many years in nearly all parts of the United States, but until recently they have not been used in areas that experienced extended periods of subfreezing temperatures. However, in recent years, air-source heat pump technology has advanced so that it now offers a legitimate space heating alternative in colder regions.
Ductless Air-Source Heat Pumps
For homes without ducts, air-source heat pumps are also available in a ductless version called a mini-split heat pump. In addition, a special type of air-source heat pump called a “reverse cycle chiller” generates hot and cold water rather than air, allowing it to be used with radiant floor heating systems in heating mode.
Geothermal Heat Pumps
Geothermal (ground-source or water-source) heat pumps achieve higher efficiencies by transferring heat between your house and the ground or a nearby water source. Although they cost more to install, geothermal heat pumps have low operating costs because they take advantage of relatively constant ground or water temperatures. Geothermal (or ground source) heat pumps have some major advantages. They can reduce energy use by 30%-60%, control humidity, are sturdy and reliable, and fit in a wide variety of homes. Whether a geothermal heat pump is appropriate for you will depend on the size of your lot, the subsoil, and the landscape. Ground-source or water-source heat pumps can be used in more extreme climates than air-source heat pumps, and customer satisfaction with the systems is very high.
Absorption Heat Pumps
A relatively new type of heat pump for residential systems is the absorption heat pump (AHP), also called a gas-fired heat pump. Absorption heat pumps use heat or thermal energy as their energy source, and can be driven with a wide variety of heat sources such as combustion of natural gas, steam solar-heated water, air or geothermal-heated water, and therefore are different from compression heat pumps that are driven by mechanical energy. AHPs are more complex and require larger units compared to compression heat pumps. The lower electricity demand of such heat pumps is related to the liquid pumping only.
Advanced Features to Look for in a Heat Pump
A number of innovations are improving the performance of heat pumps.
Unlike standard compressors that can only operate at full capacity, two-speed compressors allow heat pumps to operate close to the heating or cooling capacity needed at any particular outdoor temperature, saving energy by reducing on/off operation and compressor wear. Two-speed heat pumps also work well with zone control systems. Zone control systems, often found in larger homes, use automatic dampers to allow the heat pump to keep different rooms at different temperatures.
Some models of heat pumps are equipped with variable-speed or dual-speed motors on their indoor fans (blowers), outdoor fans, or both. The variable-speed controls for these fans attempt to keep the air moving at a comfortable velocity, minimizing cool drafts and maximizing electrical savings. It also minimizes the noise from the blower running at full speed.
Some high-efficiency heat pumps are equipped with a desuperheater, which recovers waste heat from the heat pump’s cooling mode and uses it to heat water. A desuperheater-equipped heat pump can heat water 2 to 3 times more efficiently than an ordinary electric water heater.
Another advance in heat pump technology is the scroll compressor, which consists of two spiral-shaped scrolls. One remains stationary, while the other orbits around it, compressing the refrigerant by forcing it into increasingly smaller areas. Compared to the typical piston compressors, scroll compressors have a longer operating life and are quieter. According to some reports, heat pumps with scroll compressors provide 10° to 15°F (5.6° to 8.3°C) warmer air when in the heating mode, compared to existing heat pumps with piston compressors.
Although most heat pumps use electric resistance heaters as a backup for cold weather, heat pumps can also be equipped in combination with a gas furnace, sometimes referred to as a dual-fuel or hybrid system, to supplement the heat pump. This helps solve the problem of the heat pump operating less efficiently at low temperatures and reduces its use of electricity. There are few heat pump manufacturers that incorporate both types of heat in one box, so these configurations are often two smaller, side-by-side, standard systems sharing the same ductwork.
In comparison with a combustion fuel-fired furnace or standard heat pump alone, this type of system can also be more economical. Actual energy savings depend on the relative costs of the combustion fuel relative to electricity.[6]
Geothermal Heating Boise Idaho
History of Boise’s Geothermal
Boise has used geothermal heat since the 1890s to heat Victorian homes and the original Natatorium. Back then, the cost to use the geothermal heat was just $2 a month for smaller homes and $3 a month for large homes. In 1983, the City of Boise started the beginnings of the Geothermal Heat system that is now a part of the largest, municipally-operated system in the country, heating over 90 buildings throughout downtown Boise.
How Geothermal Works
Deep below our earth’s surface runs a natural resource that the City of Boise has been utilizing for more than a century. A river of geothermally heated water flows under our city’s foothills. From heating buildings to sidewalk snowmelt and warming recreational pools, the City of Boise’s geothermal heating utility is innovative, renewable – and sustainable to the core.
How Geothermal Works
Deep below our earth’s surface runs a natural resource that the City of Boise has been utilizing for more than a century. A river of geothermally heated water flows under our city’s foothills. From heating buildings to sidewalk snowmelt and warming recreational pools, the City of Boise’s geothermal heating utility is innovative, renewable – and sustainable to the core.

Why Geothermal
Competitive Advantage
Adding this to a list of your building’s sustainability factors increases attraction, differentiation, and marketability to tenants and their employees.
Value-Driven Choice for Heating Your Building
Compared to other utility choices, geothermal is not impacted by volatility in natural gas prices. The City of Boise’s dependable heating district is powered by a completely renewable natural resource – right under our feet.
Join the Nation’s Largest Geothermal Heating Utility
Hands-on expertise from city staff can help optimize your own building’s system, while incentives make signing up easy.
Sustainable to the Core
The largest in the country, the City of Boise’s geothermal heating utility delivers the naturally heated 177° water through a network of pipes that as of 2019 warmed more than 6 million square feet of building space – a number that’s growing rapidly.
A truly closed-loop process, after the water is circulated through the heating district it’s safely added back into the aquifer.
Minimal electricity is required to power the system’s pump, with no fossil fuels used at any step in the process, this keeps the environmental impact of this resource lower than other heating options.
Where You Can Find It
Beneath the streets of Boise are over 20 miles of pipeline that heat over 6 million square feet. All over downtown, you’ll find these plaques in buildings; including JUMP, City Hall, Treasure Valley YMCA, Boise State and more.
Passive Homes
Passive solar design takes advantage of a building’s site, climate, and materials to minimize energy use. A well-designed passive solar home first reduces heating and cooling loads through energy-efficiency strategies and then meets those reduced loads in whole or part with solar energy. Because of the small heating loads of modern homes it is very important to avoid oversizing south-facing glass and ensure that south-facing glass is properly shaded to prevent overheating and increased cooling loads in the spring and fall.
Energy Efficiency First
Before you add solar features to your new home design or existing house, remember that energy efficiency is the most cost-effective strategy for reducing heating and cooling bills. Choose building professionals experienced in energy-efficient house design and construction and work with them to optimize your home’s energy efficiency. If you’re remodeling an existing home, the first step is to have a home energy audit to prioritize the most cost-effective energy efficiency improvements.
Site Selection
If you’re planning a new passive solar home, a portion of the south side of your house must have an unobstructed “view” of the sun. Consider possible future uses of the land to the south of your site—small trees become tall trees, and a future multi-story building can block your home’s access to the sun. In some areas, zoning or other land use regulations protect landowners’ solar access. If solar access isn’t protected in your region, look for a lot that is deep from north to south and place the house on the north end of the lot.
How Passive Solar Home Design Works
In simple terms, a passive solar home collects heat as the sun shines through south-facing windows and retains it in materials that store heat, known as thermal mass. The share of the home’s heating load that the passive solar design can meet is called the passive solar fraction, and depends on the area of glazing and the amount of thermal mass. The ideal ratio of thermal mass to glazing varies by climate. Well-designed passive solar homes also provide daylight all year and comfort during the cooling season through the use of nighttime ventilation.
To be successful, a passive solar home design must include some basic elements that work together:
- Properly oriented windows. Typically, windows or other devices that collect solar energy should face within 30 degrees of true south and should not be shaded during the heating season by other buildings or trees from 9 a.m. to 3 p.m. each day. During the spring, fall, and cooling season, the windows should be shaded to avoid overheating. Be sure to keep window glass clean.
- Thermal mass. Thermal mass in a passive solar home — commonly concrete, brick, stone, and tile — absorbs heat from sunlight during the heating season and absorbs heat from warm air in the house during the cooling season. Other thermal mass materials such as water and phase change products are more efficient at storing heat, but masonry has the advantage of doing double duty as a structural and/or finish material. In well-insulated homes in moderate climates, the thermal mass inherent in home furnishings and drywall may be sufficient, eliminating the need for additional thermal storage materials. Make sure that objects do not block sunlight on thermal mass materials.
- Distribution mechanisms. Solar heat is transferred from where it is collected and stored to different areas of the house by conduction, convection, and radiation. In some homes, small fans and blowers help distribute heat. Conduction occurs when heat moves between two objects that are in direct contact with each other, such as when a sun-heated floor warms your bare feet. Convection is heat transfer through a fluid such as air or water, and passive solar homes often use convection to move air from warmer areas — a sunspace, for example — into the rest of the house. Radiation is what you feel when you stand next to a wood stove or a sunny window and feel its warmth on your skin. Darker colors absorb more heat than lighter colors, and are a better choice for thermal mass in passive solar homes.
- Control strategies. Properly sized roof overhangs can provide shade to vertical south windows during summer months. Other control approaches include electronic sensing devices, such as a differential thermostat that signals a fan to turn on; operable vents and dampers that allow or restrict heat flow; low-emissivity blinds; operable insulating shutters; and awnings.
Refining the Design
Although conceptually simple, a successful passive solar home requires that a number of details and variables come into balance. An experienced designer can use a computer model to simulate the details of a passive solar home in different configurations until the design fits the site as well as the owner’s budget, aesthetic preferences, and performance requirements.
Some of the elements the designer will consider include:
- Insulation and air sealing
- Window location, glazing type, and window shading
- Thermal mass location and type.
- Auxiliary heating and cooling systems.
The designer will apply these elements using passive solar design techniques that include direct gain, indirect gain, and isolated gain.
Direct Gain
In a direct gain design, sunlight enters the house through south-facing windows and strikes masonry floors and/or walls, which absorb and store the solar heat. As the room cools during the night, the thermal mass releases heat into the house.
Some builders and homeowners use water-filled containers located inside the living space to absorb and store solar heat. Although water stores twice as much heat as masonry materials per cubic foot of volume, water thermal storage requires carefully designed structural support. An advantage of water thermal storage is that it can be installed in an existing home if the structure can support the weight.
Indirect Gain (Trombe Wall)
An indirect-gain passive solar home has its thermal storage between the south-facing windows and the living spaces. The most common indirect-gain approach is a Trombe wall.
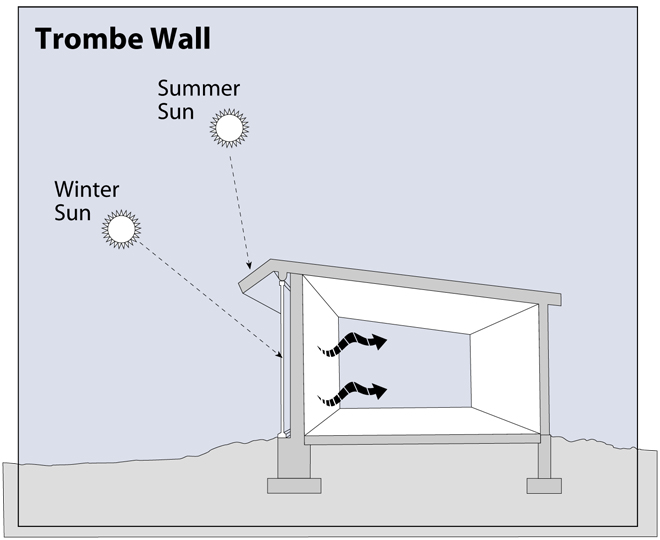
The wall consists of an 8-inch to 16-inch thick masonry wall on the south side of a house. A single or double layer of glass mounted about one inch or less in front of the dark-colored wall absorbs solar heat, which is stored in the wall’s mass. The heat migrates through the wall and radiates into the living space. Heat travels through a masonry wall at an average rate of one inch per hour, so the heat absorbed on the outside of an 8-inch thick concrete wall at noon will enter the interior living space around 8 p.m.
Isolated Gain (Sunspaces)
The most common isolated-gain passive solar home design is a sunspace that can be closed off from the house with doors, windows, and other operable openings. Also known as a sunroom, solar room, or solarium, a sunspace can be included in a new home design or added to an existing home.
Sunspaces should not be confused with greenhouses, which are designed to grow plants. Sunspaces serve three main functions — they provide auxiliary heat, a sunny space to grow plants, and a pleasant living area. The design considerations for these three functions are very different, and accommodating all three functions requires compromises.
Passive Solar Home Design for Summer Comfort
Experienced passive solar home designers plan for summer comfort as well as winter heating. A passive solar house requires careful design and siting, which vary by local climate conditions.
In most climates, an overhang or other devices, such as awnings, shutters, and trellises will be necessary to block summer solar heat gain. Landscaping can also help keep your passive solar home comfortable during the cooling season. If you are considering passive solar design for a new home or a major remodel, consult an architect familiar with passive solar techniques.[7]
The following chart provides information on energy production and consumption in the United States.
| State | Production, U.S. Share | Production, Rank | Consumption per Capita, Million Btu | Consumption per Capita, Rank | Expenditures per Capita, Dollars | Expenditures per Capita, Rank |
| WY | 6.1 | 3 | 874 | 3 | $6,703 | 1 |
| AK | 1.4 | 13 | 874 | 2 | $6,429 | 2 |
| ND | 4.5 | 7 | 804 | 4 | $6,223 | 3 |
| LA | 4 | 8 | 903 | 1 | $5,210 | 4 |
| SD | 0.3 | 37 | 447 | 8 | $4,187 | 5 |
| MT | 0.8 | 22 | 395 | 11 | $4,052 | 6 |
| IA | 1 | 16 | 479 | 5 | $3,981 | 7 |
| NE | 0.4 | 34 | 440 | 9 | $3,894 | 8 |
| WV | 5.2 | 4 | 449 | 7 | $3,759 | 9 |
| TX | 24.4 | 1 | 461 | 6 | $3,703 | 10 |
| AL | 1.3 | 14 | 366 | 13 | $3,696 | 11 |
| VT | 0 | 47 | 196 | 44 | $3,619 | 12 |
| ME | 0.1 | 44 | 268 | 28 | $3,586 | 13 |
| IN | 0.7 | 26 | 378 | 12 | $3,579 | 14 |
| MS | 0.3 | 38 | 351 | 16 | $3,578 | 15 |
| KS | 0.8 | 21 | 364 | 14 | $3,496 | 16 |
| KY | 0.8 | 23 | 354 | 15 | $3,443 | 17 |
| AR | 0.8 | 20 | 344 | 17 | $3,442 | 18 |
| NH | 0.2 | 43 | 215 | 39 | $3,354 | 19 |
| OK | 4.7 | 6 | 399 | 10 | $3,308 | 20 |
| SC | 0.8 | 24 | 299 | 20 | $3,247 | 21 |
| HI | 0 | 48 | 160 | 51 | $3,234 | 22 |
| ID | 0.2 | 42 | 298 | 21 | $3,220 | 23 |
| NM | 4.9 | 5 | 330 | 18 | $3,207 | 24 |
| CT | 0.2 | 41 | 185 | 46 | $3,205 | 25 |
| DE | 0 | 50 | 279 | 26 | $3,179 | 26 |
| WI | 0.3 | 36 | 290 | 23 | $3,139 | 27 |
| TN | 0.6 | 29 | 295 | 22 | $3,093 | 28 |
| MN | 0.5 | 31 | 303 | 19 | $3,092 | 29 |
| MO | 0.2 | 40 | 277 | 27 | $3,069 | 30 |
| MA | 0.1 | 46 | 182 | 47 | $2,977 | 31 |
| OH | 3.3 | 10 | 289 | 24 | $2,968 | 32 |
| VA | 0.9 | 18 | 263 | 29 | $2,963 | 33 |
| CA | 2.3 | 11 | 175 | 48 | $2,898 | 34 |
| GA | 0.7 | 27 | 254 | 32 | $2,892 | 35 |
| PA | 9.9 | 2 | 263 | 30 | $2,890 | 36 |
| MI | 0.7 | 28 | 259 | 31 | $2,888 | 37 |
| RI | 0 | 49 | 160 | 50 | $2,865 | 38 |
| OR | 0.5 | 33 | 232 | 36 | $2,845 | 39 |
| AZ | 0.5 | 32 | 210 | 40 | $2,834 | 40 |
| NV | 0.1 | 45 | 228 | 38 | $2,819 | 41 |
| NC | 0.8 | 25 | 236 | 35 | $2,748 | 42 |
| NJ | 0.3 | 35 | 204 | 42 | $2,675 | 43 |
| CO | 3.9 | 9 | 251 | 34 | $2,671 | 44 |
| IL | 2.3 | 12 | 283 | 25 | $2,668 | 45 |
| UT | 0.8 | 19 | 253 | 33 | $2,654 | 46 |
| MD | 0.2 | 39 | 197 | 43 | $2,584 | 47 |
| WA | 1 | 15 | 231 | 37 | $2,582 | 48 |
| DC | 0 | 51 | 208 | 41 | $2,555 | 49 |
| FL | 0.6 | 30 | 186 | 45 | $2,385 | 50 |
| NY | 0.9 | 17 | 166 | 49 | $2,380 | 51 |
Home Weatherization Assistance
The U.S. Department of Energy’s (DOE) Weatherization Assistance Program (WAP) is administered at the state and local level. To apply for weatherization assistance, contact your state weatherization agency.
How Does the WAP Application Process Work?
One of the cost effective ways to reduce heating and cooling costs is to provide caulking and weatherstripping. Therefore programs like this on are a first step and an economical step.
The following steps outline how to apply for WAP services.
Step 1: Determine Your Eligibility for Weatherization Services
One of the primary factors affecting eligibility is income. Under DOE guidelines, households at or below 200% of the poverty income guidelines are considered eligible for weatherization services or if they receive Supplemental Security Income or Aid to Families with Dependent Children. In addition, each state or territory may elect to use the U.S. Department of Health & Human Services (HHS) Low-Income Home Energy Assistance Program (LIHEAP)
The Low Income Home Energy Assistance Program (LIHEAP) helps keep families safe and healthy through initiatives that assist families with energy costs. LIHEAP provides federally funded assistance to reduce the costs associated with home energy bills, energy crises, weatherization, and minor energy-related home repairs.
LIHEAP can help you stay warm in the winter and cool in the summer through programs that reduce the risk of health and safety problems that arise from unsafe heating and cooling situations and practices.
criteria of 60% of state-median income.
WAP Grantees also give priority to the elderly, families with one or more members with a disability, families with children, or high-energy users.
Step 2: Identify Your Local Weatherization Provider
The state, tribal, or territorial website will provide a list of the local organizations or providers that offer weatherization services under its “How to Apply” section. Some states offer an online application direct from their website, but most guide you to contact the local providers. This list is usually organized by county and provides an address, phone number, and/or website.
Step 3: Complete the Weatherization Application Process
Once you have identified your local weatherization provider, contact them to start the application process. Your local provider will require proof of income for the prior year, such as pay stubs or social security payments. For information on proof of income, please refer to HHS’ Poverty Income Guidelines and Definition of Income
.Step 4: Prepare for Weatherization Services
After receiving your application and income information, your local weatherization provider will determine if you are eligible to receive weatherization services. Please remember that people who are most in need are often moved to the top of this list. Finally, if you rent, you must get permission from your landlord before workers can begin work on the house.[8]
Idaho Power Energy Audits
Idaho Power offers a discounted home energy audit, or home-performance assessment, which is a comprehensive in-home energy evaluation conducted by a certified, third-party home performance specialist (HPS). The total value of the audit is $445, but participants pay only $99 for all-electric homes and $149 for gas, propane or other fuel sourced home. It is the first step toward learning how a home uses energy. These audits are used to find areas of concern and improve the efficiency, comfort and health of a home.
From crawl space to attic, a HPS visually inspects your entire home. This includes appliances and mechanical systems, a health and safety inspection and a blower door test*, which identifies and locates air leaks. You may elect to have some energy saving improvements installed at no additional cost, if appropriate. Available improvements include installation of:
- Up to 20 energy saving light bulbs
- One high-efficiency showerhead
- Pipe wrap from the water heater to house wall – approximately 3 feet
After the audit is complete, you will understand where your home may be losing energy, what simple fixes you can do to improve efficiency and how to implement any improvements that may be needed.
*Blower door testing will not be done in homes believed to contain asbestos or vermiculite insulation.
Note: Program continuation, eligibility requirements and terms and conditions apply.
Incentives
The audit and improvements are offered at a discounted rate. The total value of the audit is $445, but participants pay only $99 for all-electric homes and $149 for gas, propane or other fuel sourced homes.
Qualifications
Existing site-built homes qualify for this program, including single family, duplexes, tri-plexes and four-plexes.
Manufactured homes, new construction or buildings with more than four units do not qualify for this program. Multifamily homes heated by a shared heating system, or that aren’t separately metered, are ineligible.
Customer Eligibility
To qualify for this program, you must:
- Be an existing Idaho Power customer.
- Live in Idaho.
- Own and occupy the home; renters may participate with prior written landlord permission.
- Be the Idaho Power account owner for the home receiving the audit.
- Use a HPS authorized by Idaho Power.[9]
- https://citation-needed-springer-com.libproxy.boisestate.edu/v2/references/10.1007/s00484-016-1214-z?format=refman&flavour=citation ↵
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4856774/ ↵
- https://iowaculture.gov/history/education/educator-resources/primary-source-sets/dust-bowl ↵
- https://www.usgbc.org/leed ↵
- https://www.usgbc.org/articles/green-building-101-what-leed ↵
- https://www.energy.gov/energysaver/heat-pump-systems ↵
- https://www.energy.gov/energysaver/passive-solar-home-design ↵
- https://www.energy.gov/eere/wap/how-apply-weatherization-assistance ↵
- https://www.idahopower.com/energy-environment/ways-to-save/savings-for-your-home/home-energy-audit/ ↵








